When you’ve had a severe reaction to a drug, it’s natural to want to avoid anything similar. But not all reactions mean you need to steer clear of an entire class of medications. Many people are told to avoid entire families of drugs after a single bad experience-only to later find out they could have safely used other options. The truth is, severe drug reaction doesn’t always mean lifelong avoidance. Knowing when to avoid a whole family-and when you don’t have to-can change your treatment options, prevent delays in care, and even save your life.
What Counts as a Severe Drug Reaction?
A severe drug reaction isn’t just a rash or upset stomach. According to the FDA, it’s an event that’s life-threatening, requires hospitalization, causes lasting disability, or leads to birth defects. These aren’t side effects you can tough out. They’re emergencies. The most dangerous reactions fall into two categories: immune-mediated (allergic) and non-immune (toxic or idiosyncratic). True allergic reactions-like anaphylaxis, hives, swelling of the throat, or difficulty breathing-happen fast, often within minutes to hours. These involve your immune system mistaking the drug for a threat. But the majority of drug reactions (80-90%) are not allergic. They’re predictable side effects: nausea from NSAIDs, dizziness from blood pressure meds, or a mild rash from amoxicillin. These don’t automatically mean you’re allergic to the whole family. The most serious non-allergic reactions are called severe cutaneous adverse reactions (SCARs). These include Stevens-Johnson syndrome (SJS), toxic epidermal necrolysis (TEN), and DRESS syndrome. TEN alone has a 30-50% death rate. If you’ve had one of these, you need to avoid the entire drug class. There’s no safe gray area. The European Medicines Agency found that 95% of TEN cases come from just six drug classes: sulfa antibiotics, anticonvulsants, allopurinol, NSAIDs, nevirapine, and corticosteroids. Avoiding these classes after a SCAR isn’t optional-it’s essential.When You Can Still Use Other Drugs in the Same Family
Here’s where things get misunderstood. Many people think a bad reaction to one drug means they can never take anything in that group. That’s often wrong. Take penicillin. For decades, people labeled "allergic to penicillin" were told to avoid all beta-lactam antibiotics-penicillins, cephalosporins, carbapenems. But research shows that 90-95% of people with this label aren’t truly allergic. A 2021 study from the American College of Allergy, Asthma, and Immunology found that only 10% of patients with a penicillin allergy history actually tested positive for IgE-mediated allergy. Many had rashes as kids that were viral, not drug-related. Others had nausea or diarrhea-side effects, not allergies. Yet they were denied life-saving antibiotics for infections like pneumonia or endocarditis. The same applies to sulfa drugs. Bactrim (sulfamethoxazole-trimethoprim) is a common culprit in SCARs. But if you had a rash from Bactrim, that doesn’t mean you can’t take sulfonamide diuretics like furosemide (Lasix) or sulfonylureas like glipizide for diabetes. The chemical structures are different. Cross-reactivity between sulfonamide antibiotics and other sulfa-containing drugs is only about 10%-and even that’s debated. NSAIDs are another example. If you had stomach bleeding from ibuprofen, you don’t need to avoid all NSAIDs. Switching to a COX-2 inhibitor like celecoxib might be safer. But if you have aspirin-exacerbated respiratory disease-where NSAIDs trigger asthma or sinus congestion-you need to avoid all traditional NSAIDs. That’s a class-wide issue because it’s based on how the drugs affect your body’s inflammatory pathways, not your immune system.Drug Families with High Cross-Reactivity Risks
Some drug classes are riskier than others. Avoiding the whole family isn’t just cautious-it’s necessary. Beta-lactam antibiotics (penicillins, cephalosporins, monobactams, carbapenems): Cross-reactivity between penicillins and cephalosporins is low-0.5% to 6.5%-but it’s higher with first-generation cephalosporins like cephalexin. If you had anaphylaxis to amoxicillin, you should avoid all beta-lactams until tested. But if you had a mild rash, you might be fine with a different one. Sulfa antibiotics: These are the biggest trigger for SCARs. If you had SJS or TEN from sulfamethoxazole, you must avoid all sulfonamide antibiotics. But again, non-antibiotic sulfa drugs (like diuretics or diabetes pills) are chemically different and usually safe. Anticonvulsants: Carbamazepine, phenytoin, lamotrigine-these are linked to DRESS and SJS, especially in people with the HLA-B*15:02 gene variant (common in Southeast Asian populations). If you had a severe reaction, avoid the entire class. Genetic testing can help identify risk before starting these drugs. NSAIDs: Avoid all traditional NSAIDs if you have aspirin-exacerbated respiratory disease. But if your reaction was just stomach upset, you might tolerate a COX-2 inhibitor or switch to acetaminophen. Allopurinol: Used for gout, it causes DRESS in about 1 in 1,000 people. If you had a severe reaction, avoid all xanthine oxidase inhibitors. The risk of recurrence is high.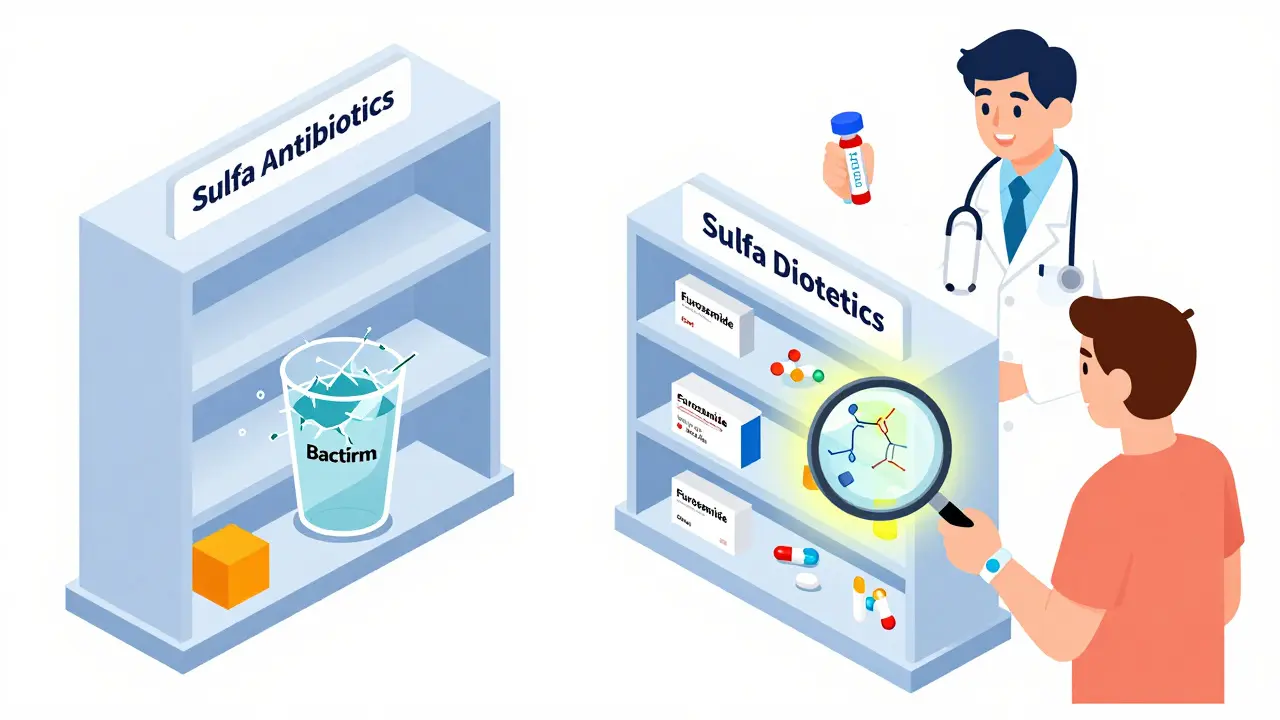
How to Know If You Really Need to Avoid a Whole Family
Don’t guess. Get evaluated. The first step is clear documentation. Was your reaction: hives? Swelling? Trouble breathing? Blistering skin? Fever? Liver failure? Each symptom points to a different mechanism. Write it down. Include timing: Did it happen within an hour? A week? The sooner the reaction, the more likely it’s immune-driven. Next, ask for an allergy evaluation. Skin testing and blood tests (like ImmunoCap Specific IgE) can now confirm true allergies with 89% accuracy-up from 60% just a few years ago. For penicillin, a skin test followed by an oral challenge under supervision can safely confirm you’re not allergic. Studies show 70-85% of people with low-risk histories pass these tests. If you had a SCAR, skip the testing. Avoid the class. But if you had a mild rash, fever, or GI upset, ask: Could this have been something else? A virus? A different drug? A food interaction? Many rashes blamed on antibiotics are actually viral.What Happens When You Avoid Too Much?
Over-avoidance isn’t harmless. It leads to delays in treatment, more expensive drugs, and higher risk of complications. A 2022 survey by the Asthma and Allergy Foundation of America found that 42% of patients with drug allergy labels faced treatment delays-on average, 3.2 days longer than needed. That might sound small, but in a serious infection, those days matter. One patient on Drugs.com described being denied antibiotics for a UTI after a past sulfa reaction, leading to sepsis. Another had to use vancomycin for a staph infection because he was labeled penicillin-allergic, even though he’d never had a true reaction. Vancomycin is more toxic, more expensive, and harder to administer. Doctors also avoid prescribing safer, more effective drugs. A 2023 study in JAMA Internal Medicine found that 32% of severe drug reactions led to inappropriate class-wide avoidance because the reaction wasn’t properly documented or understood. That’s why hospitals now use computerized systems that require physicians to justify overriding allergy alerts. At one major system, this cut inappropriate overrides by 37%.
What You Can Do Right Now
If you’ve ever had a severe reaction:- Write down exactly what happened: symptoms, timing, treatment needed.
- Ask your doctor if it was an allergy or a side effect.
- Request a referral to an allergist or immunologist for testing-especially if it was a penicillin reaction or mild rash.
- If you had a SCAR, carry a medical alert card or bracelet listing the drug class you must avoid.
- Don’t assume you’re allergic to everything in the same family. Ask: "Is this based on science-or just a label?"
What’s Changing in Drug Safety
The field is moving fast. Genetic testing now identifies people at risk before they even take a drug. For example, HLA-B*57:01 screening prevents abacavir hypersensitivity in HIV patients with 99% accuracy. The FDA approved the first component-resolved diagnostic test for drug allergy in 2022. AI tools like IBM Watson for Drug Safety are helping hospitals reduce inappropriate avoidance by 41%. More hospitals are running "penicillin de-labeling" programs. As of 2023, 87% of academic medical centers in the U.S. now offer formal allergy evaluations for patients with old penicillin labels. These programs don’t just save money-they save lives by getting patients on the right antibiotic faster. The goal isn’t to avoid drugs at all costs. It’s to avoid the right ones-and use the safe ones without fear.If I had a rash after taking penicillin, do I need to avoid all antibiotics in that family?
Not necessarily. A mild, non-itchy rash that appeared days after starting penicillin is often a viral rash, not a true allergy. True penicillin allergies cause hives, swelling, or trouble breathing within minutes to hours. About 90-95% of people labeled "penicillin allergic" can safely take penicillin or related antibiotics after proper testing. See an allergist for skin or blood tests before avoiding the whole class.
Can I take a sulfa diuretic if I had a reaction to Bactrim?
Possibly. Bactrim is a sulfonamide antibiotic. Diuretics like furosemide (Lasix) and diabetes drugs like glipizide are sulfa-containing but chemically different. Cross-reactivity is low-around 10% or less. If your reaction to Bactrim was a mild rash, you may tolerate these. But if you had Stevens-Johnson syndrome or toxic epidermal necrolysis, avoid all sulfonamides, including diuretics. Always check with your doctor or allergist.
What’s the difference between a side effect and an allergic reaction?
A side effect is a predictable, non-immune response-like nausea from NSAIDs or dizziness from blood pressure meds. An allergic reaction involves your immune system and usually includes hives, swelling, wheezing, or anaphylaxis. Allergic reactions happen quickly after exposure. Side effects can happen anytime and are often dose-related. If you’re unsure, ask for an allergy evaluation.
Are drug allergy tests accurate?
Yes, modern tests are highly accurate. Skin testing for penicillin has improved from 60% to 89% accuracy with the new ImmunoCap Specific IgE test. Blood tests and oral drug challenges under supervision can confirm whether you’re truly allergic. For non-allergic reactions like GI upset, testing isn’t useful-because it’s not an allergy. The key is matching the test to the reaction type.
If I avoid a whole drug family, will I be at risk for worse infections or complications?
Yes. Avoiding necessary antibiotics because of a mislabeled allergy can lead to longer hospital stays, use of broader-spectrum drugs like vancomycin or fluoroquinolones, and higher risk of antibiotic resistance. One study showed patients with false penicillin labels had 50% higher rates of C. difficile infection because they were given stronger, less targeted antibiotics. Getting the right diagnosis means you get the right treatment-faster and safer.
