When someone has severe pain after surgery or a broken bone, opioids can be a lifeline. But for chronic pain? They’re not the first answer-and too often, they become a trap. The truth is, opioids work. They take the edge off pain fast. But they also carry a quiet, growing danger: dependence. And once it starts, it’s not easy to walk away.
When Opioids Make Sense
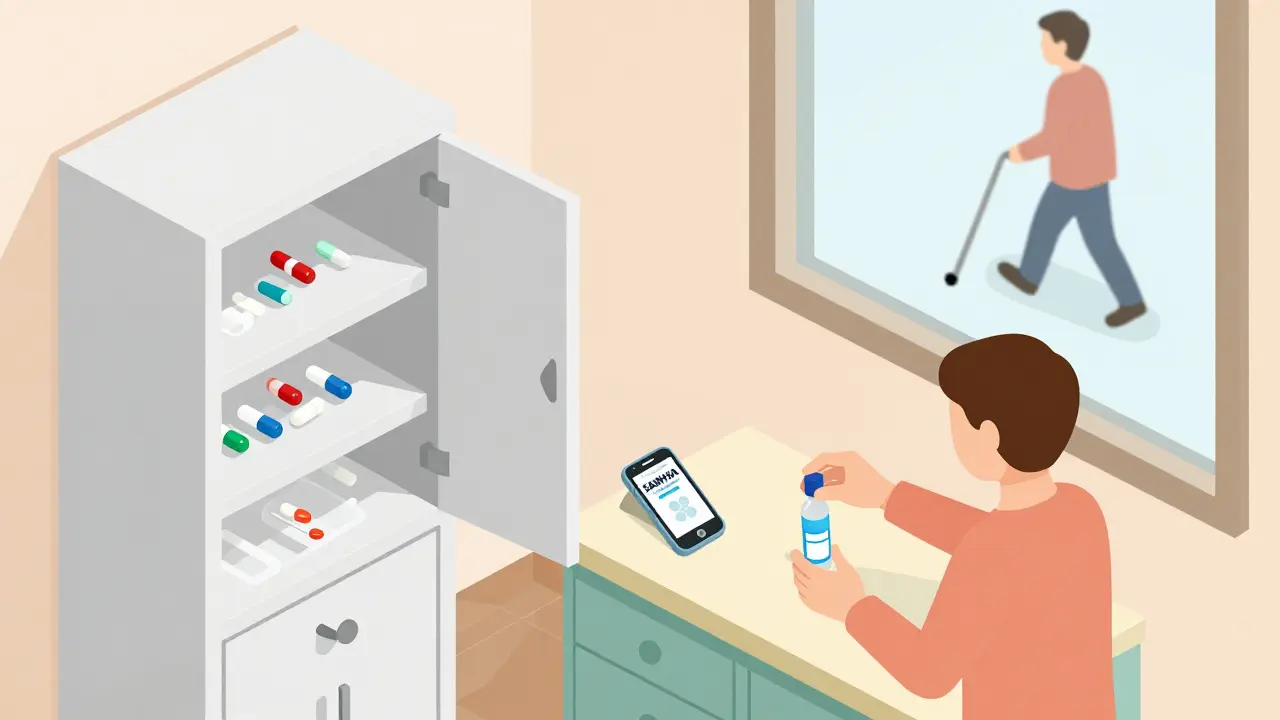
Opioids aren’t evil. They’re tools. And like any tool, they’re meant for specific jobs. The CDC’s 2022 guidelines say clearly: opioids should not be the first choice for chronic pain. That means pain lasting more than three months. For that kind of pain, physical therapy, cognitive behavioral therapy, acetaminophen, NSAIDs, or even nerve blocks come first. Opioids? They’re the backup plan. For acute pain-like after a dental procedure or a car accident-opioids can be appropriate for a few days. But even then, the goal is to use the smallest dose for the shortest time. A 2021 study found that 43% of patients prescribed opioids for acute pain got more pills than they needed. Those extra pills? They end up in medicine cabinets, where kids or visitors might find them. Or worse, they get sold. That’s not just a risk to the patient-it’s a public health problem. The real window for opioid use is when other treatments have failed, and the pain is severe enough to interfere with basic function. Think: someone with advanced arthritis who can’t walk, sleep, or get out of bed, and has tried everything else. Even then, doctors are supposed to treat it like a trial-not a lifetime prescription. If there’s no improvement in pain or function after a few weeks, the opioid should come off.The Numbers Behind Dependence
It’s easy to think, “I’m not an addict. I’m just taking my medicine.” But dependence doesn’t care about your intentions. It’s biology. The CDC says that for every 10 additional morphine milligram equivalents (MME) per day between 20 and 50 MME, the risk of overdose goes up by 8%. Between 50 and 100 MME? That risk jumps to 11% per 10 MME. So if you’re on 90 MME a day, you’re more than twice as likely to overdose as someone on 30 MME. And it’s not just dose. Combining opioids with benzodiazepines-like Xanax or Valium-multiplies the danger. The risk of overdose goes up 3.8 times. If you’re on both, your risk is nearly 11 times higher than someone taking opioids alone. That’s why many guidelines now say: if you’re on opioids and also taking a benzodiazepine, you need a plan to get off one or the other. About 8 to 12% of people prescribed opioids for chronic pain develop opioid use disorder. That number jumps to 26% for those on 100 MME or more per day. And here’s the kicker: the highest risk isn’t after months or years-it’s in the first 90 days. That’s when the brain starts rewiring itself to need the drug just to feel normal.Who’s at Highest Risk?
Not everyone who takes opioids becomes dependent. But some people are far more vulnerable. The guidelines point to five key risk factors:- Using 50 MME or more per day
- Taking benzodiazepines at the same time
- A personal or family history of substance use disorder
- Being over 65 (slower metabolism means drugs build up faster)
- Having untreated depression or anxiety

How Doctors Are Supposed to Monitor You
If you’re on opioids for more than a few weeks, your doctor isn’t supposed to just write a prescription and forget about you. There’s a checklist:- Pain level (on a scale of 0 to 10)
- How well you’re functioning (can you walk? sleep? work?)
- Urine drug tests to check for other substances
- Screening tools like the Current Opioid Misuse Measure to spot red flags
- Checking your state’s prescription drug monitoring program (PDMP) to see if you’re getting pills from other doctors
What Happens When You Need to Stop
Stopping opioids suddenly is dangerous. It can trigger severe withdrawal: nausea, sweating, muscle cramps, anxiety, insomnia. Worse, it can push people back toward street drugs like heroin or fentanyl because the pain returns worse than before. Tapering is the answer-but it has to be done right. There are three approaches:- Slow taper: Reduce dose by 2-5% every 4 to 8 weeks. Best for people who are stable and getting some benefit.
- Moderate taper: 5-10% every 4 to 8 weeks. For people whose pain hasn’t improved or who’ve developed tolerance.
- Rapid taper: 10% per week. Only for those on 90+ MME/day or showing signs of harm.
What’s Changing Now
The opioid crisis hasn’t gone away-but the response is evolving. Between 2012 and 2020, opioid prescriptions in the U.S. dropped by 42.5%. That’s because doctors are learning. PDMPs are now used in 49 states, and 87% of prescriptions are checked against them before being filled. New pain treatments are coming fast. The NIH’s HEAL Initiative has poured $1.5 billion into research since 2018. Right now, 37 non-addictive pain drugs are in late-stage clinical trials. Some target nerve signals. Others use immune pathways. None of them have the same risk of dependence. Still, in 2021, over 80,000 people died from opioid overdoses. That’s more than ever before. Why? Because fentanyl has taken over the illegal market. It’s 50 to 100 times stronger than morphine. A tiny amount can kill. And if you’ve been on prescription opioids for years, your tolerance is lower than you think.What You Can Do
If you’re on opioids:- Ask your doctor: “Is this still helping me function better?”
- Know your daily dose in MME. If you’re over 50, ask about naloxone.
- Never mix with alcohol, sleep meds, or anxiety pills.
- Store pills locked up. Throw away unused ones at a take-back site.
- If you feel like you can’t stop, or you’re craving them-talk to someone. There’s help.
- Watch for changes in behavior: secrecy, mood swings, sleep issues.
- Keep naloxone in the house. It’s available without a prescription in most states.
- Don’t shame. Support. Encourage professional help.
It’s Not About Fear. It’s About Balance.
Opioids have a place in medicine. But they’re not a cure. They’re a temporary tool. And using them wisely means knowing when to start-and when to stop. The goal isn’t to eliminate all opioid use. It’s to make sure no one suffers needlessly from pain… and no one loses their life to a pill they thought was safe.Are opioids ever safe for long-term pain?
Yes-but only in rare cases where non-opioid treatments have failed, and the benefits clearly outweigh the risks. Most people with chronic pain don’t need them. Those who do should be closely monitored, kept on the lowest effective dose, and regularly re-evaluated. Long-term use should never be automatic.
Can I become addicted even if I take opioids exactly as prescribed?
Yes. Addiction and dependence are not the same as misuse. Dependence means your body adapts to the drug-you may have withdrawal if you stop. Addiction involves compulsive use despite harm. About 8-12% of people on long-term opioid therapy develop opioid use disorder, even when following their doctor’s instructions. Genetic factors play a big role, and it’s not a sign of weakness.
What should I do if I think I’m dependent on opioids?
Don’t stop suddenly. Talk to your doctor about a tapering plan. You can also reach out to a substance use specialist or call the SAMHSA helpline at 1-800-662-4357. Medication-assisted treatments like buprenorphine or methadone can help manage withdrawal and reduce cravings. Recovery is possible-and it’s not a failure of willpower.
Why are doctors prescribing fewer opioids now?
Because the data changed. In the 1990s and early 2000s, opioids were overprescribed based on weak evidence and aggressive marketing. By 2010, overdose deaths were rising fast. The CDC’s 2016 and 2022 guidelines shifted the standard: opioids are no longer first-line for chronic pain. Doctors now use risk tools, PDMPs, and safer alternatives. Prescriptions have dropped 42.5% since 2012-not because pain is gone, but because safer options exist.
Is it true that naloxone is available without a prescription?
Yes. In most U.S. states, naloxone can be bought over the counter at pharmacies without a prescription. Some states even distribute it for free through public health programs. It’s safe, easy to use, and can save a life. If you or someone you know is on opioids, having naloxone on hand is as important as having a fire extinguisher.
What are the best alternatives to opioids for chronic pain?
Physical therapy, exercise, cognitive behavioral therapy (CBT), acupuncture, and certain antidepressants or antiseizure meds (like duloxetine or gabapentin) are proven to help. For joint pain, injections like corticosteroids or hyaluronic acid can work. New non-opioid drugs are in trials, including ones that block pain signals without affecting the brain’s reward system. Many people find relief through a combination of these-not just one.
