When Your Generic Medication Doesn’t Work, Insurance Won’t Always Help
You’ve been told to switch from your brand-name drug to the generic version. It’s cheaper. It’s FDA-approved. It’s supposed to be the same. But after a few weeks, your symptoms are worse. Your blood work is off. You’re having side effects you never had before. When you call your insurance to ask for your original medication back, they say no-generic is available, so that’s what you get.
This isn’t rare. It happens to thousands of people every month. And it’s not because the system is broken-it’s because the rules don’t always match real life.
Why a Generic Can Fail Even When It’s "Bioequivalent"
The FDA says generics must deliver 80% to 125% of the active ingredient compared to the brand-name drug. That sounds precise. But for some medications, that 45% window is huge.
Think about drugs like levothyroxine (for thyroid), warfarin (a blood thinner), or antiseizure meds like levetiracetam. These have what’s called a narrow therapeutic index. That means the difference between a dose that works and one that causes harm is tiny. A 10% variation in absorption can mean the difference between stable thyroid levels and a heart attack. Or between no seizures and a full-blown episode.
Studies show 15-20% of patients on these types of drugs have trouble with generics. It’s not about the active ingredient being wrong-it’s about fillers, coatings, or how the pill breaks down in your gut. Your body might process one generic differently than another. Or than the brand.
One patient on Reddit tracked her TSH levels after switching from Synthroid to a generic. They jumped from 2.1 to 14.7 in eight weeks. Her doctor called it a "therapeutic failure." Her insurance called it "not medically necessary."
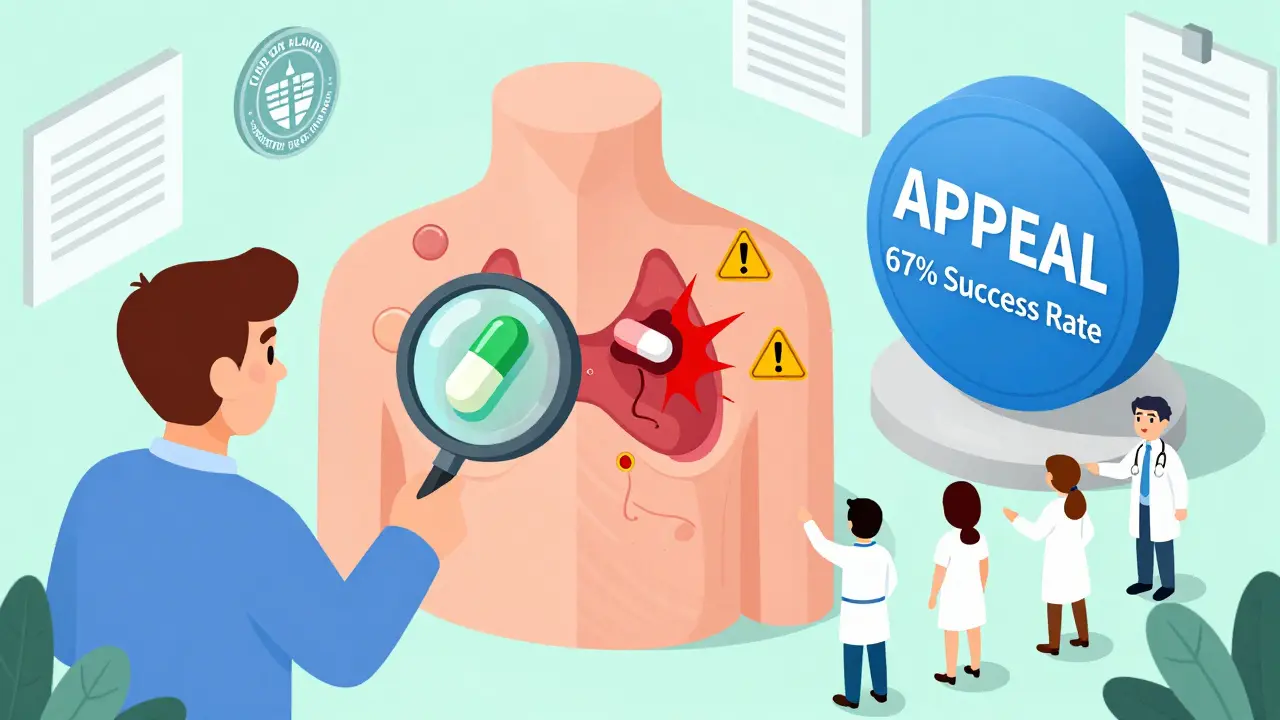
The Appeal Process Isn’t Optional-It’s Your Right
Insurance companies can deny your brand-name drug, but you’re not stuck with their answer. The Affordable Care Act and state laws give you the right to appeal. And you’re more likely to win than you think.
Here’s how it works:
- Get your denial letter. It should list the reason-often code DA2000 ("generic available"). Keep it. You’ll need it.
- Call your doctor. Don’t wait. Ask them to write a letter explaining why the generic doesn’t work for you. This isn’t just a note. It needs specifics: dates, symptoms, lab results, previous attempts with other generics.
- File an internal appeal. You have 180 days for commercial plans, 60 days for Medicare Part D. Use the form on your insurer’s website or mail it in. Attach everything: lab reports, medication logs, pharmacy records.
- If denied again, request an external review. This is where most wins happen. An independent doctor reviews your case. The Patient Advocate Foundation found 67% of these appeals succeed when documentation is strong.
Medicare patients have five levels of appeal, including review by the Office of Medicare Hearings and Appeals. It’s long, but it’s there. And under the Inflation Reduction Act, if you win, you don’t pay the higher cost for the brand-name drug during the process.
What Makes an Appeal Succeed
Most appeals fail because they’re vague. "I don’t feel well on the generic" won’t cut it.
Successful appeals include:
- Lab values showing clear changes-like rising TSH, INR, or drug blood levels.
- Medication logs with dates, symptoms, and dosages.
- A physician letter that cites clinical guidelines (like the Endocrine Society’s stance on thyroid meds) and explains why the brand is medically necessary.
- Proof of prior failures-if you tried two other generics and both failed, mention that. Some states require this.
One study found appeals with detailed pharmacokinetic explanations had an 82% approval rate. Those with just a short note? 37%.
Insurers sometimes demand you try three or four generics before approving the brand. But 28 states now ban that practice if you’ve already documented failure. Check your state’s rules.
Who Helps You Win
You don’t have to do this alone.
GoodRx’s Appeal Assistant walks you through a template letter your doctor can sign in minutes. Over 147,000 people used it in 2023. It’s free. It’s simple.
The Patient Advocate Foundation offers free case managers. They help pull records, write letters, and track deadlines. Their 2023 report showed 92% satisfaction among users.
Specialty pharmacies like OptumRx and Accredo now have appeal teams built into their services. If your doctor prescribes through them, ask if they handle appeals. Their success rate? 73%-compared to 51% for patients who do it themselves.
Nonprofits like the Crohn’s & Colitis Foundation and Epilepsy Foundation have downloadable appeal toolkits. They include exact templates for your condition.
Why This Keeps Happening
Generics make up 90% of prescriptions but only 23% of drug spending. Insurers save millions by pushing them. That’s why they fight hard to deny brand-name requests.
But here’s the catch: when generics fail, patients end up in the ER, hospitalized, or unable to work. The JAMA Internal Medicine journal estimates $28 billion a year is spent on avoidable hospitalizations because of therapeutic failures.
That’s why states are changing the rules. California, New York, and Texas now approve brand-name drugs after one documented failure. The 2024 Consolidated Appropriations Act requires insurers to show real-time benefit info-so your doctor knows upfront if a drug will be denied.
And the FDA is moving too. Their 2023 draft guidance suggests evaluating bioequivalence on a patient-by-patient basis. That could change everything.
What to Do Right Now
If you’re stuck:
- Find your denial letter. Look for the code.
- Call your doctor’s office. Ask for a 30-minute slot just to talk about your appeal. Bring your symptom log.
- Download a template from the Patient Advocate Foundation or Epilepsy Foundation.
- Use GoodRx’s Appeal Assistant to draft your letter.
- Submit your appeal within 30 days. Don’t wait.
Don’t assume your doctor will fight for you. Most are overworked. But if you give them the right paperwork, they’ll sign it. They’ve seen this before.
You’re not asking for luxury. You’re asking for your body to work the way it should.
Frequently Asked Questions
What if my insurance says there’s no proof the generic didn’t work?
Insurers often claim there’s "no clinical evidence"-but that’s usually because you haven’t given them the right evidence. Start tracking your symptoms and lab results the moment you switch. Take blood tests before and after. Write down every side effect, every flare-up, every time you feel worse. Your doctor can use this to show a clear pattern. Courts and reviewers accept this data. You just have to collect it.
Can I switch back to the brand if I’ve already tried two generics?
Yes, and in 28 states, insurers are legally required to approve it. Even if you’re in a state without this law, you can still appeal. The key is documenting that each generic failed. For example, if you tried two different levothyroxine generics and both caused your TSH to spike, that’s two documented failures. The Crohn’s & Colitis Foundation says this is often enough to win.
How long does the appeal process take?
Internal appeals take 14-30 days. External reviews take 30-45 days. But if your condition is urgent-like seizures, heart issues, or uncontrolled diabetes-you can request an expedited review. Medicare and many commercial plans must respond in 72 hours. Tell them your life is at risk. That triggers faster processing.
What if my doctor won’t help me write the letter?
Some doctors are overwhelmed. But most will sign if you bring them a pre-written template. Use the ones from the Patient Advocate Foundation or Epilepsy Foundation-they’re designed to be easy to sign. If your doctor refuses, ask for a referral to a specialist who’s more familiar with appeals. Sometimes, a neurologist or endocrinologist’s letter carries more weight than a primary care doctor’s.
Is it worth appealing for antidepressants or pain meds?
It’s harder, but still possible. Unlike thyroid or seizure meds, these don’t have clear lab markers. But you can still win by documenting changes in your daily life: sleep patterns, ability to work, mood logs, hospital visits, ER trips. A 2023 study showed appeals for antidepressants succeeded 45% of the time when patients included detailed symptom tracking. It’s not easy, but if your quality of life is crashing, it’s worth trying.
Next Steps and Troubleshooting
If you’ve been denied and don’t know where to start:
- Go to patientadvocate.org and use their free appeal tool.
- Call 1-800-532-5274 for a free case manager.
- Check your state’s insurance department website for formulary exception rules.
- Ask your pharmacy if they offer appeal support.
If you’re on Medicare, visit medicarerights.org for step-by-step guides.
Don’t give up after one denial. The system is slow, but it works-if you push. 68% of people get denied the first time. But 52% eventually win. You’re not alone. And you’re not wrong.
