When your doctor prescribes a brand-name drug, you might expect to get exactly what’s written on the prescription. But more often than not, the pharmacy hands you a different pill - cheaper, smaller, maybe a different color - with the same active ingredient. That’s generic substitution. It’s not a mistake. It’s policy. And if you don’t understand how it works, you could end up paying more, feeling worse, or both.
Why Insurance Companies Push Generic Substitution
Insurance companies don’t care about brand names. They care about cost. And generics save them - and you - a lot of money. In the U.S., generics make up 90% of all prescriptions but only 18% of drug spending. That’s a $373 billion annual savings for the whole healthcare system, according to the Association for Accessible Medicines. For your insurer, switching you from Lipitor to atorvastatin isn’t a suggestion. It’s a rule. Most private insurers, like Blue Cross, Aetna, and UnitedHealthcare, have mandatory generic programs. If you choose the brand-name version, you pay the difference out of pocket. That means if your brand costs $120 and the generic is $25, you’re on the hook for $95. For people on tight budgets, that’s not just inconvenient - it’s a barrier to treatment. But here’s the catch: these rules aren’t the same everywhere. In Texas, a pharmacist can’t substitute unless three conditions are met: the generic is cheaper, you don’t say no, and your doctor didn’t write “dispense as written.” In California, you have to be told about the substitution before it happens. In New York, the pharmacist must document it. And in some states, even if your doctor says “no substitution,” the insurer will still pay only for the generic - and you’ll cover the rest.What the Law Actually Says (And Doesn’t Say)
There’s no single federal law controlling generic substitution. Instead, you’re stuck in a patchwork of 50 state laws, plus federal guidelines from the FDA. The FDA says generics are just as safe and effective as brand-name drugs - same active ingredient, same strength, same way of taking it. They must prove bioequivalence: their blood levels must fall within 80-125% of the brand’s. That’s not a guess. It’s science. But the law doesn’t always match the science. In 19 states, pharmacists are required to substitute generics unless the doctor says otherwise. In seven states and Washington, D.C., you have to give explicit consent before the switch. In 31 states, you just get a notice - no signature needed. And in 24 states, pharmacists have no legal protection if something goes wrong after a substitution. That means if you have a bad reaction, they could be sued - even if they followed the rules. The biggest loophole? The “dispense as written” note. If your doctor writes that on the prescription, most states will honor it. But many doctors don’t know they need to do it. Or they think it’s optional. It’s not. If you need the brand, you have to make it clear - in writing - before the prescription leaves the office.When Generic Substitution Can Go Wrong
Most of the time, switching to a generic works perfectly. But not always. The biggest complaints come from patients on drugs with a narrow therapeutic index - drugs where even a small change in blood level can cause serious problems. Think warfarin (blood thinner), lithium (for bipolar disorder), or levothyroxine (for hypothyroidism). One Reddit user, u/MedPatient87, switched from Synthroid to generic levothyroxine and spent six months with fluctuating thyroid levels. Three dose adjustments. Three blood tests. All because the generic, while technically bioequivalent, had different inactive ingredients that affected absorption. That’s not rare. A 2022 Drugs.com analysis found that 24% of negative reviews blamed inconsistent generic manufacturing. Different companies use different fillers, dyes, or coatings. For most people, it doesn’t matter. For some, it does. Another issue: biologics. These aren’t simple pills. They’re complex proteins made from living cells - like insulin, Humira, or Enbrel. The FDA allows “biosimilars” as cheaper versions, but they’re not true generics. They’re “highly similar,” not identical. And substitution rules are even stricter. In 38 states, you must be notified before a biosimilar is swapped in. In 27, you need to give consent. And in many cases, your doctor has to re-prescribe it specifically.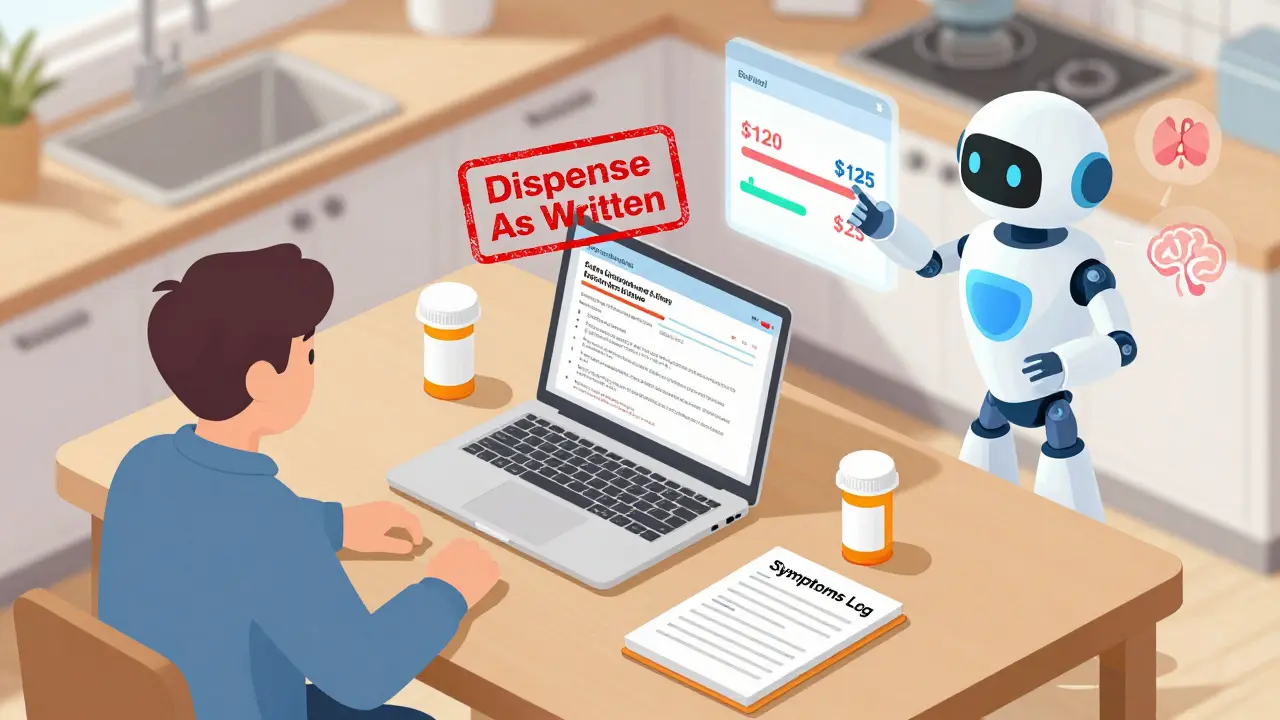
How to Keep Your Brand-Name Drug (Legally)
If you’ve had a bad reaction to a generic, or your condition is unstable, you have rights. Here’s how to fight back:- Get your doctor to write “Dispense as Written” or “Brand Medically Necessary” on the prescription. This is the most direct way. It’s not a request. It’s a legal instruction.
- Ask for prior authorization. Most insurers require this for brand-name drugs. Your doctor submits documentation - like lab results showing your levels didn’t stabilize on the generic - and the insurer reviews it. Blue Cross Blue Shield of Michigan approved 78% of these requests in 2023 when medical evidence was clear.
- Know your insurance’s formulary. Check your plan’s drug list. If the brand isn’t covered at all, you can’t get it unless you pay full price. If it’s covered with high copays, you can still get it - but you’ll pay more.
What Pharmacists Are Required to Do (And What They Won’t Tell You)
Pharmacists are on the front lines. They’re trained to substitute when allowed. But many don’t explain the process. You might not even know you were switched until you get the bill. Here’s what they’re legally required to do:- In 31 states: notify you that a substitution occurred - even if it’s just on the receipt.
- In 19 states: substitute automatically unless told not to.
- In 9 states: use the FDA’s “Orange Book” to confirm therapeutic equivalence. That’s the official list of which generics are approved as interchangeable.
- In all states: they cannot substitute if the prescription says “do not substitute” - unless your insurer overrides it.

What You Can Do Right Now
You don’t need to wait for your next appointment to protect yourself. Here’s your action plan:- Check your prescription. Does it say “dispense as written”? If not, ask your doctor to add it.
- Read your pharmacy receipt. Look for the generic name. If it’s different from what your doctor wrote, you were substituted.
- Call your insurer. Ask: “What’s your policy on generic substitution for [medication name]?” Get it in writing.
- Track your symptoms. If you feel different after switching - fatigue, dizziness, mood swings - log it. Take a photo of your pill. Save your receipt. This is evidence if you need to appeal.
- Ask for the Orange Book. If your pharmacist says a generic is interchangeable, ask to see the FDA’s listing. Not all generics are created equal.
The Bigger Picture: Why This Matters
Generic substitution isn’t just about saving money. It’s about control. Who decides what you take - your doctor, your pharmacist, or an insurance algorithm? The system is designed to cut costs, not to personalize care. And while most people benefit from lower prices, others get caught in the middle - switching back and forth, adjusting doses, living with uncertainty. The solution isn’t to ban generics. It’s to make the system fairer. Doctors need better training on how to write prescriptions that protect patients. Pharmacists need clearer guidelines. And patients need to know their rights before they walk into the pharmacy. If you’re on a life-sustaining medication - thyroid, epilepsy, heart, mental health - don’t assume the system has your back. Ask questions. Document everything. And never let cost be the only deciding factor in your treatment.Can my pharmacist substitute my brand-name drug without telling me?
In 31 U.S. states and Washington, D.C., pharmacists are required to notify you when they substitute a generic for a brand-name drug. In the other 19 states, substitution is automatic unless your doctor writes "dispense as written." In seven states, you must give explicit consent before the switch. Always check your receipt - the generic name should be listed. If you’re unsure, ask the pharmacist directly.
What if I feel worse after switching to a generic?
If you notice new side effects, changes in symptoms, or lab results that don’t match your previous levels, document everything - dates, symptoms, pill appearance. Contact your doctor immediately. You may need to switch back to the brand. Most insurers will approve a return to the brand if you provide medical evidence of failure with the generic. This is called a "therapeutic failure" exception.
Can my doctor stop a generic substitution?
Yes - but only if they write "Dispense As Written" or "Brand Medically Necessary" directly on the prescription. This is a legal instruction in most states. However, some insurers still try to override it by making you pay the full price difference. If your doctor refuses to write this note, ask them to explain why - and consider getting a second opinion if your condition is unstable.
Are all generics the same?
No. While all generics must contain the same active ingredient and meet FDA bioequivalence standards, they can be made by different manufacturers with different inactive ingredients - like fillers, dyes, or coatings. For most people, this doesn’t matter. But for those sensitive to additives (e.g., people with allergies or malabsorption issues), switching between generic brands can cause problems. Always note which generic manufacturer you’re taking and report any changes to your pharmacist or doctor.
Why do some drugs have no generic version?
Some drugs are still under patent protection. Others are too complex to copy easily - like inhalers, injectables, or biologics. Biosimilars (the generic version of biologics) require years of extra testing and are approved under stricter rules. As of 2023, there are over 10,000 small-molecule generics but only 38 biosimilars in the U.S. market. That means many high-cost medications still have no affordable alternative.
Does Medicare cover brand-name drugs if I want them?
Yes - but you’ll pay more. Medicare Part D plans have formularies that favor generics. If you request a brand-name drug when a generic is available, you’ll pay the difference between the brand and generic price. You can still get it, but you’re responsible for the extra cost. If you’ve already tried the generic and it didn’t work, you can file an exception request with your plan using medical documentation.
