Have you ever looked up at a clear blue sky and seen dark specks drifting across your vision? Or caught a sudden flash of light out of the corner of your eye, like a spark or a lightning bolt, even when you’re in a dim room? You’re not alone. These moments - called floaters and flashes - are incredibly common, especially as we get older. But while most are harmless, some can signal something serious. Knowing the difference could save your sight.
What Are Floaters and Flashes?
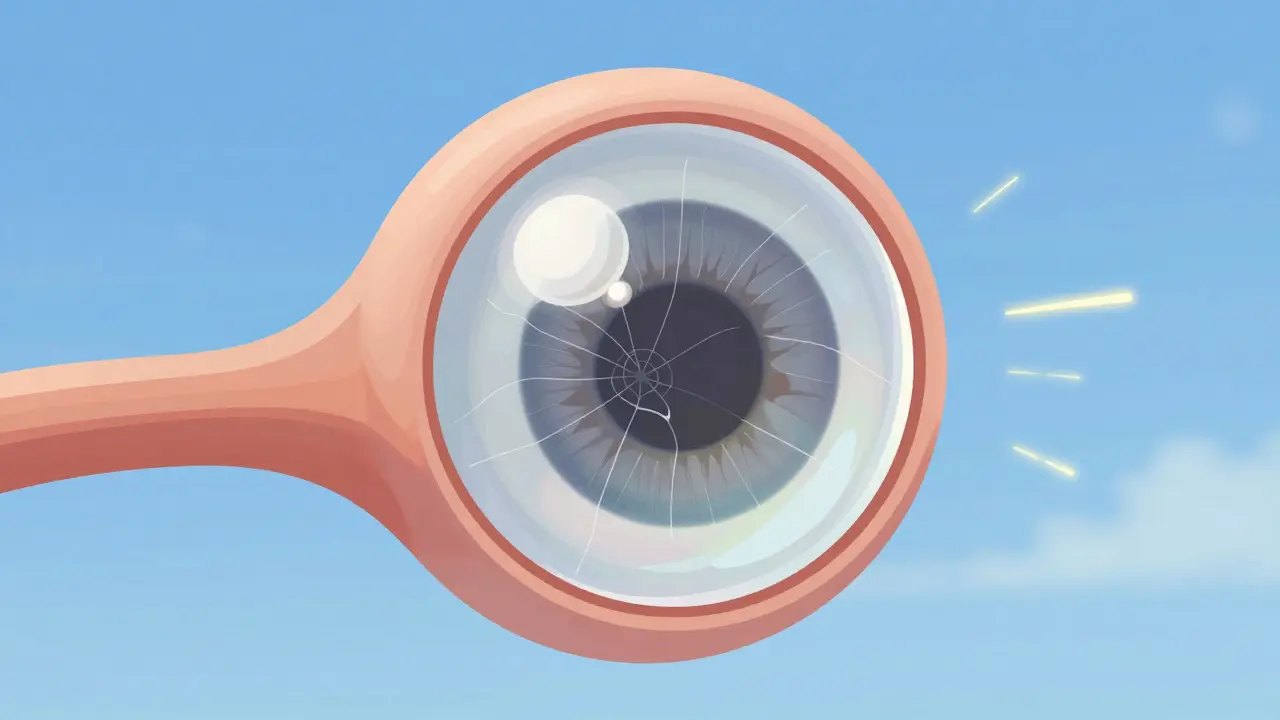
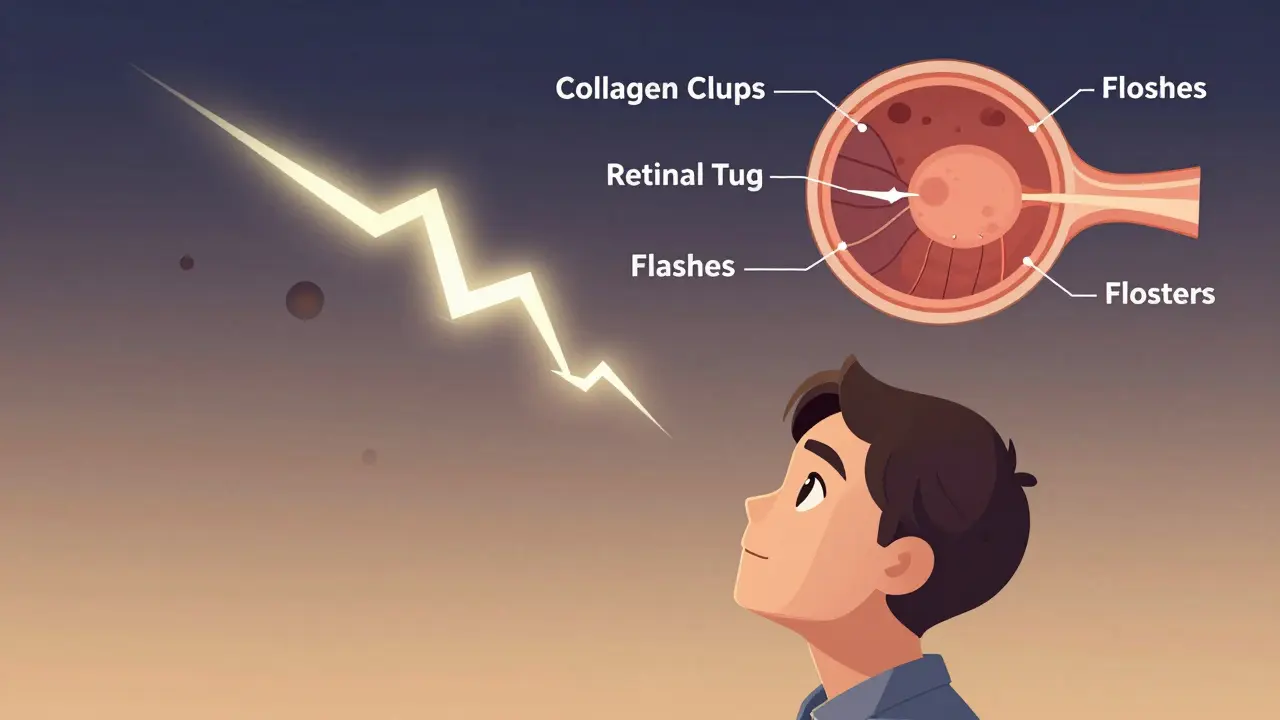
Floaters are those little shapes that seem to swim in front of your eyes. They look like dots, cobwebs, threads, or tiny bugs. They move when you move your eyes and seem to dart away when you try to focus on them. Flashes, on the other hand, are brief streaks or sparks of light - often seen in your peripheral vision - that appear without any actual light source. They can feel like a camera bulb going off, or like static on an old TV screen.
Both are caused by changes in the vitreous humor - the clear, gel-like substance that fills the space between your lens and retina. At birth, this gel is thick and firm, holding your eyeball’s shape. But as you age, it starts to break down. Around age 40 to 50, the collagen fibers inside the vitreous begin to clump together and shrink. This process, called vitreous syneresis, turns the gel into more of a liquid. Eventually, the vitreous pulls away from the retina - a normal event called posterior vitreous detachment (PVD).
When the vitreous tugs on the retina during this detachment, it can cause flashes. The retinal cells fire off signals, and your brain interprets them as light. Meanwhile, clumps of collagen cast shadows on the retina - these are your floaters. It’s not that anything is wrong with your eyes. It’s just physics: debris floating in a gel that’s turning to liquid.
How Common Are They?
Very. By age 65, about 75% of people have experienced floaters. Nearly two-thirds of those over 70 will have had a posterior vitreous detachment. If you’re nearsighted, you’re more likely to see them earlier - sometimes as young as 30 - because longer eye shape increases traction on the retina. The risk goes up even more if you’ve had eye surgery, trauma, or inflammation.
What’s surprising is how few people realize this is normal. Many panic the first time they notice a sudden shower of floaters or repeated flashes. But in most cases, PVD is just part of aging - like gray hair or wrinkles. The problem comes when it’s not PVD.
When Is It Something Worse?
Here’s the critical point: Floaters and flashes alone don’t mean you’re losing your vision. But sudden changes might.
Benign PVD usually causes:
- A single shower of new floaters - not dozens, not hundreds
- Flashes that last a few days to weeks, then fade
- No loss of vision or dark curtain over your sight
- Symptoms in only one eye
But if you notice any of these, get checked within 24 hours:
- Sudden increase in floaters - like a handful of black specks appearing at once
- Flashes that keep happening, especially in clusters
- A dark shadow or curtain moving across your vision
- Loss of side vision (peripheral vision)
- Blurry or distorted central vision
These signs point to a retinal tear or retinal detachment. When the vitreous pulls too hard on the retina, it can rip a small hole. Fluid then slips through, lifting the retina off the back of the eye. That’s retinal detachment - and it can cause permanent blindness if not treated fast.
Studies show that 70% of cases with vitreous hemorrhage (blood in the vitreous) linked to PVD involve a retinal tear. And if you’re under 50 and suddenly get floaters or flashes, it’s far less likely to be normal aging. It could mean diabetes, uveitis, trauma, or another condition that needs treatment.
What Happens at the Eye Doctor?
There’s no home test. You can’t diagnose this yourself. That’s why experts - from Duke Health to the Royal Australian College of General Practitioners - all say the same thing: Any new onset of floaters or flashes needs a dilated eye exam.
A good ophthalmologist will:
- Dilate your pupils with drops - this takes about 20 minutes
- Use a special lens to look directly at your retina
- Check for tears, holes, bleeding, or detachment
- Assess your peripheral vision and pupil response
This exam is painless. You might see spots afterward from the dilation, but that fades in a few hours. The goal isn’t to treat PVD - it’s to rule out the dangerous stuff. If everything looks normal, you’re likely fine. If there’s a tear, laser surgery or cryotherapy can seal it before detachment happens.
Can You Treat Floaters?
Most people don’t need treatment. The brain adapts. Over six months to a year, floaters tend to sink out of your central vision. You learn to ignore them. That’s why many don’t even mention them to their doctor - until they get flashes.
Some clinics offer laser treatment (vitreolysis) to break up large floaters. But it’s not widely covered by insurance, carries risks like retinal damage, and isn’t proven effective for everyone. Surgery to remove the vitreous (vitrectomy) is even riskier and reserved only for severe cases. For 99% of people, observation is the best approach.

What Can You Do?
There’s no way to prevent PVD. It’s natural aging. But you can reduce risks:
- If you have diabetes, keep your blood sugar under control - high glucose damages eye blood vessels
- Wear protective eyewear during sports or home projects
- Don’t ignore symptoms - even if you’ve had PVD before, new changes need checking
- Know your family history - if relatives had retinal detachments, be extra vigilant
And remember: if you’re worried, go get checked. Anxiety is normal. But waiting too long isn’t.
Real-Life Signs to Watch For
One patient in Bristol, 68, noticed a few new floaters after reading in bed. She thought it was just tired eyes. Two days later, she saw flashes every time she turned her head. She waited a week - then got scared. By the time she saw her optometrist, she had a small retinal tear. Laser treatment that same day prevented detachment. She’s now back to gardening without worry.
Another man, 52, had flashes for three days. He thought it was stress. He didn’t go to the doctor. Two weeks later, he lost half his peripheral vision. He had a full retinal detachment. Surgery saved his central sight, but he’ll never regain the lost side vision.
These aren’t rare stories. They’re common outcomes of delayed care.
Are floaters and flashes always a sign of something serious?
No. Most floaters and flashes are caused by posterior vitreous detachment (PVD), a normal part of aging. They’re harmless if they appear gradually, fade within weeks, and don’t come with vision loss. But sudden increases in floaters, persistent flashes, or shadows across your vision need immediate evaluation.
How long do floaters last?
Floaters from PVD usually become less noticeable over 3 to 6 months as the brain adapts and the debris settles. Some may linger for a year or longer, but they rarely worsen. If they suddenly increase in number or change shape, it’s not normal - get checked.
Can floaters cause blindness?
Floaters themselves don’t cause blindness. But they can be a warning sign. If they’re caused by a retinal tear or detachment, and that’s left untreated, permanent vision loss can occur. That’s why it’s not the floater you need to fear - it’s what might be causing it.
Should I go to the ER for floaters and flashes?
Not necessarily. Go to an eye specialist - an optometrist or ophthalmologist - within 24 to 48 hours. If you have sudden vision loss, a dark curtain, or severe pain, go to the ER. Otherwise, a dedicated eye clinic can do the full retinal exam faster than an emergency room can.
Is there a way to prevent floaters?
You can’t prevent the natural aging of the vitreous. But managing conditions like diabetes, avoiding eye trauma, and wearing UV-blocking sunglasses may reduce risks of complications like bleeding or inflammation that can worsen floaters. Regular eye exams are your best defense.