Anticoagulation Risk Calculator
See if stroke risk outweighs bleeding risk when you're on blood thinners. This tool uses evidence-based data from major medical guidelines.
Stroke Risk Assessment
This score measures your stroke risk. 2+ for men, 3+ for women = high stroke risk
Bleeding Risk Assessment
This score measures bleeding risk. 3+ = higher bleeding risk
Typical range: 0-10 falls per year for older adults
Risk Comparison Results
Stroke risk is 8.75x higher than bleeding risk
Based on evidence from the American College of Physicians and European Society of Geriatric Medicine
The data shows: Stroke risk without anticoagulation is typically 8-10x higher than bleeding risk from falls. This means continuing anticoagulation is almost always safer for preventing strokes.
Every year, more than 1 in 3 adults over 65 falls. For someone on a blood thinner-like warfarin or a DOAC-that fall isn’t just a stumble. It’s a potential emergency. But here’s the truth most doctors still get wrong: fall risk alone should never stop you from taking a blood thinner if you need it. The fear of bleeding from a fall is real. But the risk of having a stroke because you skipped your medication? That’s often far worse.
Why Stopping Blood Thinners Over Fall Risk Is a Dangerous Mistake
Many clinicians, especially in nursing homes or geriatric clinics, see a patient who’s unsteady on their feet and automatically think: “Better not give them a blood thinner.” It feels safer. But it’s not. Studies show that for older adults with atrial fibrillation (AF), the annual stroke risk without treatment is 1.5% to 3%. For someone with a CHA2DS2-VASc score of 3 or higher-that’s the standard tool doctors use to measure stroke risk-that risk jumps to over 3% per year. That’s roughly 1 in 30 people having a stroke each year. Now, compare that to the risk of a serious brain bleed from a fall while on a blood thinner. It’s only 0.2% to 0.5% per year. That’s less than 1 in 200. And here’s the kicker: you’d need to fall nearly 300 times in one year for the bleeding risk to outweigh the stroke prevention benefit of warfarin. Most people don’t fall even 10 times a year. The American College of Physicians, the European Society of Geriatric Medicine, and the American Heart Association all agree: do not withhold anticoagulation just because someone falls. In fact, they’ve made it a formal “Things We Do for No Reason” campaign-meaning it’s a common but harmful practice that needs to stop.DOACs Are the Smart Choice for Fall-Prone Patients
If you’re on a blood thinner and you’re at risk of falling, your best option isn’t warfarin. It’s a DOAC-direct oral anticoagulant. These include apixaban, rivaroxaban, dabigatran, and edoxaban. They’re not just easier to take (no weekly blood tests), they’re safer. DOACs reduce the risk of intracranial hemorrhage (bleeding in the brain) by 30% to 50% compared to warfarin. That’s huge for someone who might trip down the stairs or slip in the bathroom. A brain bleed is often fatal or disabling. A stroke from AF can be, too-but DOACs cut your chance of that happening by 60% to 70%. In the U.S., about 80% of new anticoagulant prescriptions for AF are now DOACs. Why? Because doctors are finally catching on. For patients over 75, with balance issues, or living in a care home, DOACs are the clear winner.Don’t Use CHA2DS2-VASc Alone-Check the HAS-BLED Score Too
CHA2DS2-VASc tells you your stroke risk. HAS-BLED tells you your bleeding risk. You need both. CHA2DS2-VASc scores: 2 or higher in men, 3 or higher in women? You’re in the moderate-to-high stroke risk group. Anticoagulation is recommended. HAS-BLED scores: If you score 3 or higher, you have a higher bleeding risk. But that doesn’t mean don’t take a blood thinner. It means you need to be more careful. Check your blood pressure. Review your medications. Fix your home. Get your vision tested. Treat your anemia. These are fixable risks. Many people think a high HAS-BLED score means “no anticoagulation.” That’s outdated. The guideline says: “High HAS-BLED = more monitoring, not no treatment.”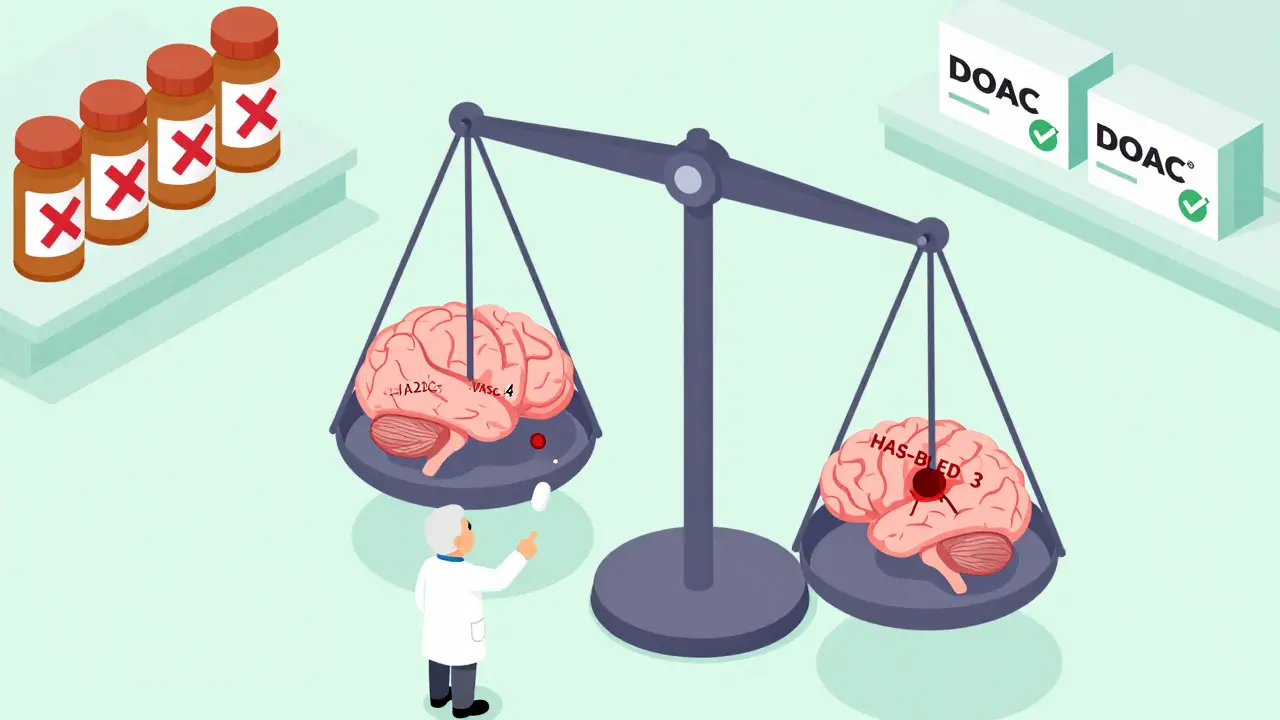
What Actually Reduces Fall Risk (And Why It Matters More Than Stopping Medication)
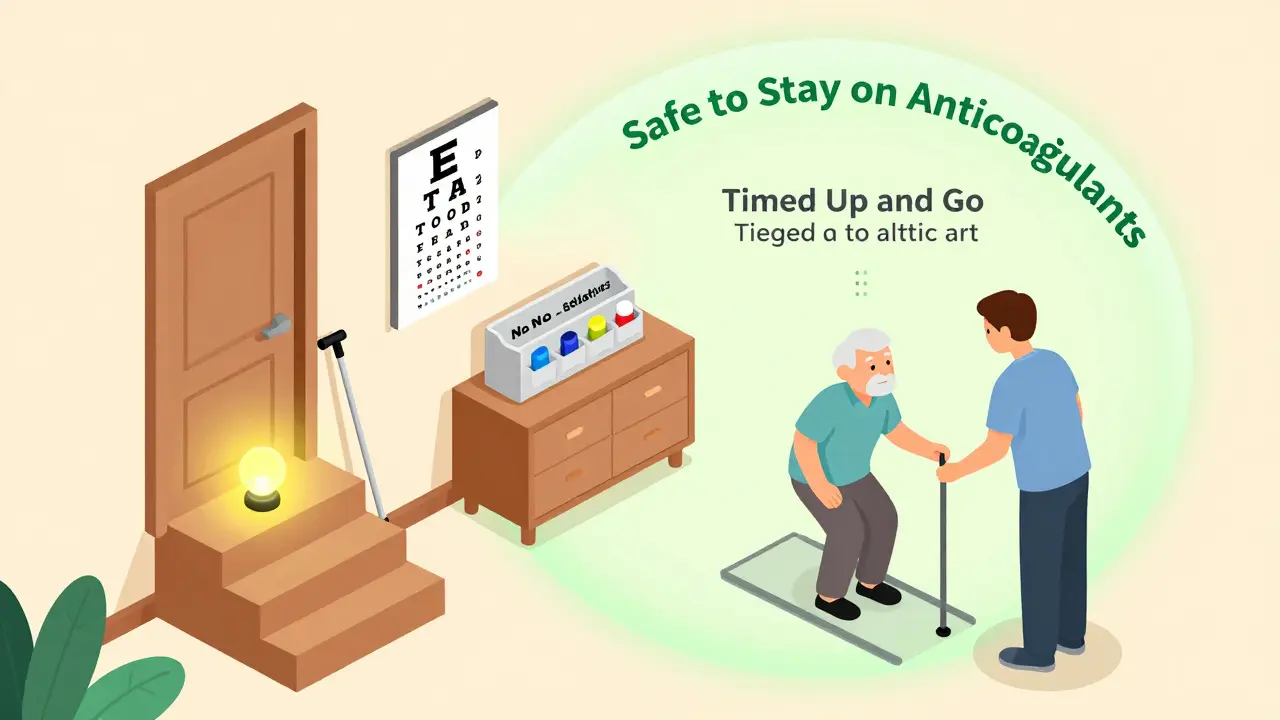
Instead of taking away your blood thinner, fix what’s making you fall. That’s the real solution. Here’s what works:- Review your meds. Sedatives, sleeping pills, antidepressants, and even some blood pressure drugs can make you dizzy. Ask your doctor: “Can any of these be stopped or lowered?”
- Test your balance. The Timed Up and Go test takes 30 seconds. You stand up from a chair, walk 3 meters, turn, walk back, and sit down. If it takes more than 12 seconds, you’re at high fall risk. Physical therapy can help.
- Fix your home. Loose rugs, poor lighting, no grab bars in the bathroom-these are easy fixes. Install nightlights. Remove clutter. Use a shower chair.
- Check your eyes. Cataracts, glaucoma, or outdated glasses? Get them fixed. Vision is a top cause of falls.
- Treat low blood pressure when standing. If you feel lightheaded when you stand up, that’s orthostatic hypotension. It’s common in older adults and easily managed with hydration, compression stockings, or adjusting meds.
What You Should Never Do
There are three dangerous myths you need to avoid:- “I’ll just take a lower dose of my DOAC.” Wrong. Studies show reducing DOAC doses doesn’t lower bleeding risk-it raises stroke risk. These drugs are already dosed for safety in older adults. Don’t mess with it.
- “I’ll keep my INR lower than normal.” That’s for warfarin users. Keeping INR below 2.0 doesn’t prevent bleeds. It lets clots form. Your stroke risk goes up. Don’t do it.
- “I’ll stop the blood thinner if I fall once.” One fall doesn’t mean you’re unsafe. It means you need a falls assessment. Don’t panic. Don’t quit.
When Might It Be Right to Skip Anticoagulation?
There are rare cases where avoiding blood thinners makes sense:- You have active bleeding-like a stomach ulcer or recent brain bleed.
- Your blood pressure is uncontrolled-above 180/110.
- You have a severe bleeding disorder, like hemophilia.
- You’re very frail, with life expectancy under 1-2 years, and your stroke risk is low (CHA2DS2-VASc = 1 or 2).
What to Do Next
If you or a loved one is on a blood thinner and has fallen-or is afraid of falling-here’s your action plan:- Ask your doctor: “What’s my CHA2DS2-VASc score?” If it’s 2+ (men) or 3+ (women), you need anticoagulation.
- Ask: “What’s my HAS-BLED score?” If it’s 3+, we’ll work on reducing modifiable risks.
- Request a full falls assessment: meds review, balance test, home safety check, vision test.
- Ask: “Can I switch to a DOAC?” If you’re on warfarin, DOACs are safer and easier.
- Don’t stop your medication without a plan. Talk to your doctor. Don’t self-decide.
Final Thought: Safety Isn’t About Avoiding Risk-It’s About Managing It
You can’t eliminate every fall. But you can prevent a stroke. You can’t control aging. But you can control your environment, your meds, and your choices. The goal isn’t to live in a bubble. It’s to live well, safely, and without fear. For most people on anticoagulants, that means staying on them-while fixing what’s making them fall.Don’t let fear of a fall steal your future. Talk to your doctor. Get assessed. Stay protected.
Should I stop my blood thinner if I fall once?
No. One fall doesn’t mean you’re unsafe. It means you need a falls assessment. Stopping your blood thinner increases your stroke risk. Instead, work with your doctor to find out why you fell-was it dizziness, poor lighting, a medication side effect? Fix those, and you can stay on your anticoagulant safely.
Are DOACs safer than warfarin for people who fall?
Yes. DOACs reduce the risk of bleeding in the brain by 30% to 50% compared to warfarin. They’re also easier to use-no regular blood tests. For older adults at risk of falling, DOACs are the recommended first-line treatment for atrial fibrillation, unless you have severe kidney problems or a mechanical heart valve.
Can I lower my DOAC dose to reduce bleeding risk?
No. Studies show reducing DOAC doses doesn’t lower bleeding risk-it increases stroke risk. DOACs are already dosed for safety in older adults. Off-label dose reduction is not recommended by any major guideline. If you’re worried about bleeding, talk to your doctor about switching from warfarin to a DOAC instead.
What if my doctor says I can’t take a blood thinner because I fall too much?
Ask for evidence. The American College of Physicians, the American Heart Association, and the European Society of Geriatric Medicine all say fall risk alone is not a reason to avoid anticoagulation. Request a CHA2DS2-VASc score calculation. If it’s 2 or higher (men) or 3 or higher (women), you need anticoagulation. Ask for a referral to a geriatric specialist or falls clinic if your doctor is unsure.
How can I reduce my risk of falling while on anticoagulants?
Start with four steps: 1) Review all your medications with your doctor-cut unnecessary sedatives or blood pressure drugs. 2) Get a balance test like the Timed Up and Go. 3) Fix your home: add grab bars, remove rugs, install nightlights. 4) Get your eyes checked. Physical therapy for balance and strength training can reduce falls by up to 40%.
