Emotional Blunting Treatment Estimator
Treatment Effectiveness Estimator
See expected improvement rates for common emotional blunting solutions based on clinical studies
Select an option above to see expected improvement rate.
Important: These rates are based on clinical studies. Always consult your doctor before making any medication changes.
Timeline: It takes 4-6 weeks for emotional responses to return after treatment changes.
It’s supposed to help you feel better. But for many people taking SSRIs, something strange happens: they don’t feel much at all. Not sadness. Not joy. Not even the quiet comfort of a warm cup of tea or the laughter of a friend. Instead, there’s just… nothing. This isn’t rare. It’s not a myth. It’s called emotional blunting, and it affects between 40% and 60% of people taking SSRIs like sertraline, escitalopram, or fluoxetine. If you’ve noticed you’re not crying at movies anymore, or your dog’s excited greeting doesn’t spark a smile, you’re not alone-and you’re not broken.
What Emotional Blunting Actually Feels Like
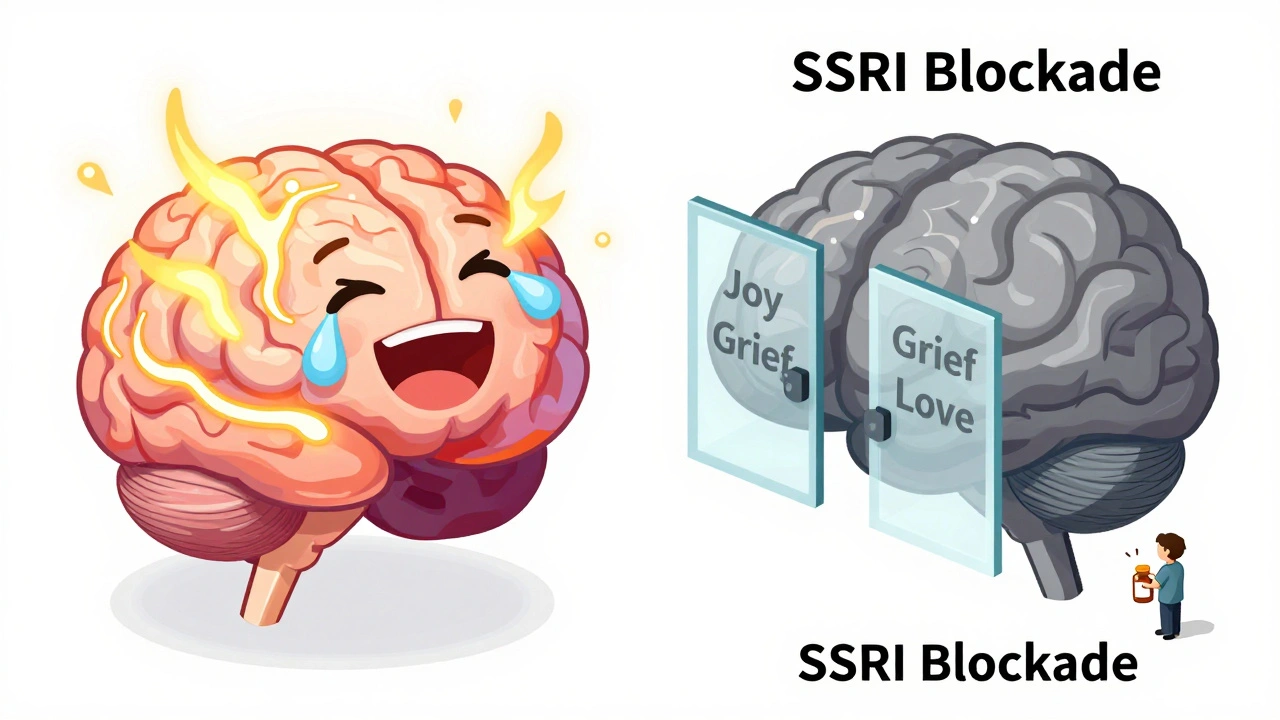
Emotional blunting isn’t just being tired or stressed. It’s a flattening of your entire emotional world. People describe it as living behind glass. You can see the world moving around you-birthdays, funerals, weddings, quiet mornings-but you’re no longer part of it. You don’t feel the sting of grief, the rush of excitement, or even the warmth of love. Some say they can still recognize emotions intellectually-they know they’re supposed to feel sad at a funeral-but the feeling itself is gone.This isn’t just about sadness. It’s about everything. Joy fades. Anger disappears. Even the small pleasures-eating your favorite food, hearing a song you love-lose their spark. One woman on Reddit wrote: "I stopped crying at sad movies and didn’t feel joy when my dog greeted me-just a flat nothing." That’s not depression returning. That’s the medication changing how your brain processes emotion.
Studies from Cambridge and Copenhagen show SSRIs interfere with something called reinforcement learning-the brain’s way of learning from rewards and consequences. When this system slows down, everything feels less meaningful. Your brain stops assigning value to experiences. That’s why you don’t feel motivated to do things you used to love. It’s not laziness. It’s neurochemistry.
Why It’s So Common-and Why Doctors Miss It
SSRIs work by increasing serotonin in the brain. That helps some people get out of the deepest pits of depression. But serotonin doesn’t just control sadness. It also regulates how we experience pleasure, connection, and emotional depth. When you flood the system, you don’t just turn down the pain-you turn down the volume on everything.Doctors know this happens. But they rarely ask about it. A 2022 survey found only 38% of psychiatrists routinely screen for emotional blunting. Most focus on whether the patient is less suicidal or sleeping better. If you’re not crying all day, they assume the medication is working. But emotional blunting doesn’t show up on a PHQ-9 score. It shows up in your relationships, your creativity, your sense of self.
And it’s not just you. The NHS reported over 8.3 million antidepressant prescriptions in England in 2021/22. If even half of those users experience some level of blunting, that’s millions of people living in emotional gray.
It’s Not Just SSRIs-But They’re the Main Culprit
Not all antidepressants do this. Bupropion (Wellbutrin) affects dopamine and norepinephrine, not serotonin. Studies show only about 33% of people on bupropion report emotional blunting-significantly lower than SSRIs. In one 2022 meta-analysis of over 1,200 patients, switching from an SSRI to bupropion improved emotional blunting in 72% of cases.Mirtazapine and agomelatine also have lower rates, though data is more limited. Vortioxetine shows promise, but most studies were funded by the manufacturer, so results need more independent verification. The key takeaway: if you’re feeling emotionally numb, switching within the SSRI family won’t help. Escitalopram, sertraline, fluoxetine-they all work the same way. The problem isn’t the drug. It’s the class.
What to Do When You Feel Nothing
If you’re experiencing emotional blunting, you have options. But you don’t have to choose between feeling terrible and feeling nothing.1. Talk to your doctor about lowering your dose. Many people take the highest dose because they think "more is better." But emotional blunting is dose-dependent. A 2021 review found reducing your SSRI dose by 25-50% improved emotional responsiveness in 68% of cases. You might still get the benefits for depression without the numbness.
2. Consider switching to bupropion. This is the most evidence-backed option. A 2022 study in the Journal of Clinical Psychiatry showed 72% of people saw improvement after switching from an SSRI to bupropion. Some doctors combine the two-keeping a low dose of SSRI while adding bupropion. This approach worked for 63% of patients in clinical practice.
3. Don’t quit cold turkey. Stopping SSRIs suddenly can cause withdrawal symptoms like dizziness, brain zaps, nausea, and even anxiety spikes. Withdrawal affects 28-80% of people, depending on the drug. Always taper slowly under medical supervision. It takes 4-6 weeks for emotional responses to return after a change.
4. Ask for screening. Bring this up at your next appointment. Ask: "Could my emotional numbness be from the medication?" If your doctor brushes it off, ask for a referral to a psychopharmacologist. This isn’t weakness. It’s your brain asking for help.
When Emotional Blunting Might Be a Good Thing
Some people say the numbness saved them. During the worst of their depression, they couldn’t get out of bed. Crying all day. Overwhelmed by every emotion. For them, SSRIs brought a kind of peace. "I needed the numbness to function," one person wrote on a patient forum. And that’s valid.There’s no one-size-fits-all. If you were suicidal, paralyzed by panic, or drowning in despair, then a flat emotional state might have been the price of survival. That doesn’t make it ideal-but it makes it understandable.
The problem isn’t that SSRIs work. The problem is that we treat emotional blunting like a side effect instead of a core feature. We don’t warn people. We don’t measure it. We don’t offer alternatives until it’s too late.
The Bigger Picture: Are We Missing Something?
Some experts argue emotional blunting isn’t just from the medication-it’s leftover depression. Dr. John Krystal points out that people who still feel emotionally flat after months on SSRIs might not be fully recovered. That’s a fair point. But here’s the catch: if your depression symptoms have improved but your emotions haven’t returned, that’s not recovery. That’s partial healing.And it’s getting worse. Antidepressant prescriptions in England rose 6.7% in one year. The global market hit $14.7 billion in 2022. Meanwhile, the European Medicines Agency added emotional blunting to SSRI labels in 2022 after patient pressure. The National Institute of Mental Health just funded a $4.2 million study to find biomarkers for this effect. We’re starting to see it as a real problem.
But we’re still treating it like a footnote. We need better tools. We need doctors who ask the right questions. We need patients who know they have a right to feel-fully, deeply, even if it hurts.
What’s Next?
New antidepressants are in development. Twelve of the 17 drugs currently in Phase III trials are designed specifically to avoid emotional blunting. Some target serotonin receptors more precisely. Others use entirely different pathways. The first might be available by 2026.In the meantime, you don’t have to wait. If you’re feeling emotionally flat, it’s not your fault. It’s not weakness. It’s a known effect of the medication you’re taking. And you have choices.
Ask for a dose reduction. Ask about bupropion. Ask for a second opinion. You deserve to feel the full range of being human-not just the absence of pain, but the presence of joy, grief, anger, and love. The numbness isn’t peace. It’s a stopgap. And you don’t have to live in it forever.
