Why Exercise Can Drop Your Blood Sugar Too Low
Working out is one of the best things you can do for diabetes. It helps your body use insulin better, lowers blood sugar, and improves energy. But for many people with diabetes-especially those on insulin-it comes with a scary risk: low blood sugar.
When you move, your muscles grab glucose from your blood without needing insulin. That’s great-until your blood sugar drops too far. If it falls below 70 mg/dL, you might feel shaky, sweaty, dizzy, or confused. In severe cases, it can lead to passing out or seizures. About half of people with type 1 diabetes avoid exercise because they’re afraid of this happening.
The problem doesn’t stop when you finish your workout. Your body stays more sensitive to insulin for up to three days after exercise. That means your blood sugar can crash hours later-even while you’re sleeping. Nighttime lows after afternoon workouts are one of the most common and dangerous issues.
Check Your Blood Sugar Before You Start
Never jump into a workout without checking your blood sugar first. The American Diabetes Association says you should test 15 to 30 minutes before you begin. If your reading is below 90 mg/dL, you’re in the danger zone. At this point, you need to eat something before you even lace up your shoes.
Here’s what to aim for:
- Below 90 mg/dL: Eat 0.5 to 1.0 gram of carbs per kilogram of body weight (for a 70 kg person, that’s 35-70g of carbs).
- Between 90-150 mg/dL: Eat 15-20 grams of fast-acting carbs like glucose tablets, juice, or fruit.
- Above 150 mg/dL: You’re likely safe to start, but keep monitoring.
Some experts, like Dr. Anne Peters, suggest going even higher-150 to 180 mg/dL-if you’re doing high-intensity exercise like sprinting or heavy lifting. This gives you a buffer so you don’t dip too low mid-workout.
What to Eat Before and During Exercise
Not all carbs are the same. For quick action, go for glucose tablets, fruit juice, or honey. Avoid fat or protein-heavy snacks like peanut butter or cheese-they slow down absorption. You need something that hits your bloodstream fast.
If your workout lasts longer than 30 minutes, keep eating. Every 30 to 60 minutes, take another 15-20 grams of carbs. That’s about one banana, half a sports drink, or four glucose tabs. Even if you feel fine, don’t skip this. Your blood sugar can drop suddenly, especially during steady activities like cycling or swimming.
Many people find it helpful to carry a small snack bag with glucose tabs, dried fruit, and a water bottle. Keep it in your gym bag, your car, or even your pocket. You never know when you’ll need it.
Timing Your Insulin Matters More Than You Think
If you use insulin, the timing of your dose can make or break your workout. Exercising when your insulin is peaking? That’s a recipe for a low. Most rapid-acting insulin peaks 1 to 2 hours after injection. So if you take a bolus at 11 a.m. and hit the gym at noon, you’re asking for trouble.
The fix? Exercise at the same time every day. Consistency helps your body predict how your blood sugar will react. If you always work out at 5 p.m., your body learns to expect it.
Also, check your insulin-on-board (IOB). This is how much active insulin is still working in your system. If you have 2 units of insulin still active and you start running, your body might process it like 3 or 4 units because exercise boosts insulin sensitivity. That’s why the T1D Exchange says IOB is one of the top predictors of exercise lows.
If you use an insulin pump, set a temporary basal rate reduction. Lower your basal by 50-75% starting 60 to 90 minutes before exercise. If you’re on injections, reduce your pre-workout bolus by 25-50%, depending on intensity and duration.
Not All Workouts Are Created Equal
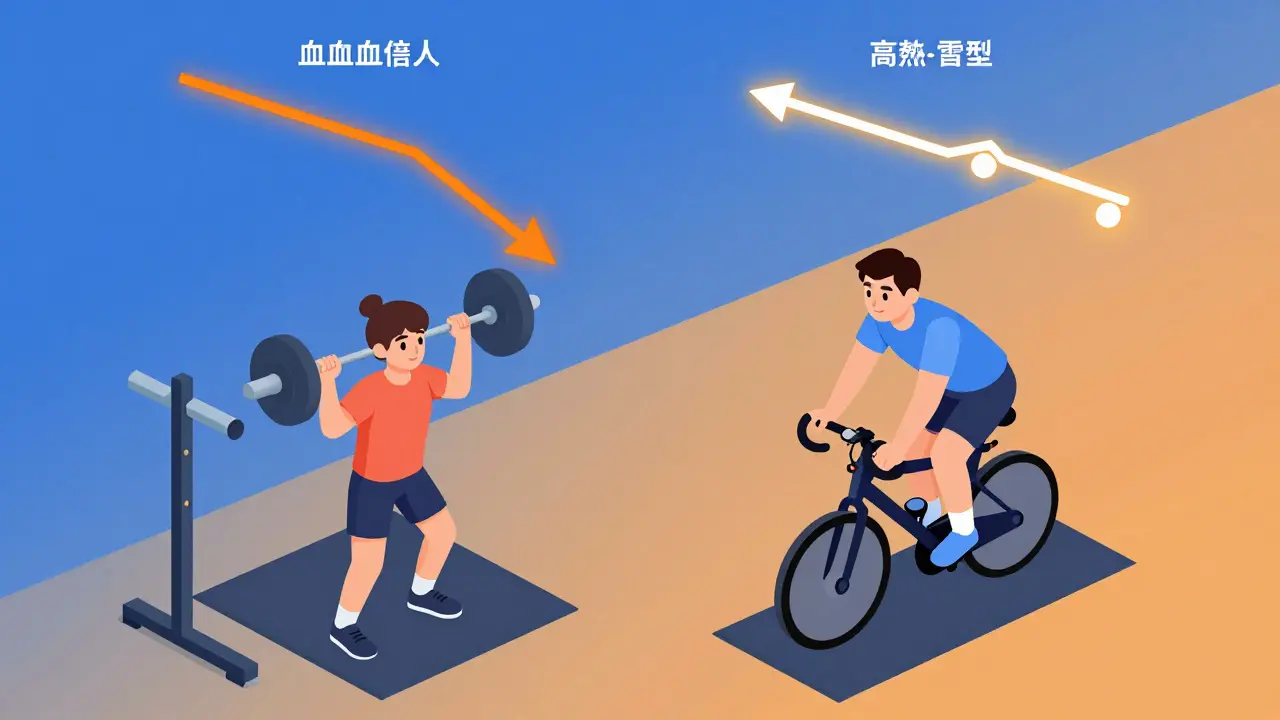
Here’s something surprising: not every type of exercise drops your blood sugar. Aerobic workouts-like jogging, cycling, or swimming-tend to lower glucose steadily. But resistance training and high-intensity bursts? They can actually raise it.
Studies show that doing 10 seconds of all-out sprinting before or after your main workout can block the drop. One person on Reddit said adding a quick bike sprint before his 30-minute ride cut his lows from four times a week to once every two weeks.
Strength training is another game-changer. Doing 45 minutes of weightlifting before a 45-minute cardio session reduced glucose drops from 61 mg/dL to just 36 mg/dL in one study. Even better, the effect lasts. Your muscles keep pulling glucose from your blood for hours after lifting.
High-intensity interval training (HIIT) works similarly. Short bursts of sprinting or burpees followed by rest periods keep blood sugar stable during and after exercise. A 2019 study found HIIT lowered hypoglycemia risk for up to 45 minutes after stopping.
So if you’re always getting lows during cardio, try switching things up. Do weights first. Add sprints. Mix in short bursts of intensity. Your blood sugar will thank you.
Use Your CGM Like a Pro
Continuous glucose monitors (CGMs) are no longer luxury tools-they’re essential for safe exercise. In 2022, 68% of people with type 1 diabetes using CGMs checked their glucose before working out. Only 42% of non-CGM users did.
Modern CGMs like Dexcom G7 have an “exercise mode” that lowers alert thresholds by 20 mg/dL during activity. That means you get warnings earlier, giving you time to react. But don’t rely on alerts alone. Glucose can drop faster than the device updates.
Set your CGM to notify you every 15 minutes during exercise. That way, you’re not guessing. If your trend arrow is pointing down hard, eat now-even if your number is still above 90.
Also, watch your trend. A slow, steady drop is easier to manage than a sudden plunge. If your glucose is falling 2-3 mg/dL per minute, you’re in trouble. Eat immediately.
Watch Out for Delayed Lows (Especially at Night)
The biggest hidden danger? Lows that happen hours after you finish. Up to 70% of people with type 1 diabetes experience delayed hypoglycemia-often during sleep. That’s why you can feel fine after a workout, go to bed, and wake up at 4 a.m. with a shaking hand and a reading of 52 mg/dL.
How to prevent it:
- Check your glucose before bed. If it’s below 120 mg/dL, eat a snack with 15g carbs and a little protein-like a slice of whole grain toast with peanut butter or a small cup of yogurt.
- Don’t skip your bedtime check, even if you worked out in the morning.
- If you used a lot of insulin during the day, consider a small basal reduction overnight.
Many people on forums like Beyond Type 1 report at least one severe nighttime low per month tied to daytime exercise. It’s not rare. It’s expected. Plan for it.

What to Do If You Get a Low During Exercise
If your blood sugar drops below 70 mg/dL while you’re working out, stop. Immediately. Don’t try to “push through.”
Follow the 15-15 rule:
- Eat 15 grams of fast-acting carbs.
- Wait 15 minutes.
- Check again.
If it’s still low, repeat. Don’t resume exercise until your glucose is above 100 mg/dL and stable. Even then, go easy. Your body is still recovering.
Always carry your glucose source with you. Don’t assume your gym has snacks. Don’t rely on someone else to help you. Keep tabs, juice, or candy in your pocket, your bag, your bike handlebar-wherever you can reach it fast.
It Takes Time to Get It Right
There’s no one-size-fits-all rule. What works for one person might cause a low for another. It takes 3 to 6 months of tracking, testing, and adjusting to truly understand how your body responds to different workouts.
Start slow. Try one new activity at a time. Write down:
- What you ate and when
- Your insulin doses
- Your blood sugar before, during, and after
- How you felt
Over time, patterns emerge. You’ll notice that swimming drops your sugar more than cycling. That lifting weights in the morning keeps you stable, but doing it after dinner causes a crash.
And remember: it’s okay to have a low. It doesn’t mean you failed. It means you’re learning. Every time you catch it early, adjust, and recover, you’re getting better at managing your diabetes-not just surviving it, but thriving.
What’s Coming Next
The future of exercise and diabetes is getting smarter. In March 2023, the Tandem t:slim X2 pump got FDA approval for an “Exercise Impact” feature that uses AI to predict glucose drops and automatically reduces insulin. Clinical trials are now testing dual-hormone artificial pancreases that deliver both insulin and glucagon during workouts-cutting lows by over half.
By 2026, experts predict nearly all diabetes devices will include built-in exercise management. That’s huge. But even with all this tech, your own knowledge and habits still matter most. The machines help. You decide when to eat, when to stop, and when to push.
