When a patient walks into your office and asks, "Is the generic version really the same as the brand?" - you need more than reassurance. You need hard data. And the data is clear: for the vast majority of patients, generic medications deliver the same clinical results as their brand-name counterparts. But not everyone believes it. Some providers still hesitate. Some patients refuse. Why? Because myths persist. Let’s cut through the noise with what the science actually shows.
How Generics Are Proven to Work
Every generic drug approved in the U.S. must pass a strict test called bioequivalence. It’s not a formality. It’s a rigorous scientific process. The FDA requires generics to deliver the same active ingredient, in the same amount, at the same rate as the brand-name drug. That means the body absorbs it the same way. The standard? The concentration of the drug in the bloodstream must fall within 80% to 125% of the brand-name drug’s levels. For most drugs, that’s a tight enough window to guarantee identical effects. For drugs with a narrow therapeutic index - like warfarin, levothyroxine, or tacrolimus - the rules are even stricter. Studies using scaled average bioequivalence (SCABE) look at how patients respond over time, not just a single dose. A 2020 study in Nature Scientific Reports tracked transplant patients switching between brand and generic tacrolimus over six weeks. No clinically meaningful differences in blood levels or rejection rates were found. That’s not luck. That’s science.What Real-World Studies Show
The most convincing evidence doesn’t come from lab tests. It comes from millions of real patients. A landmark 2019 study in PLOS Medicine analyzed over 1.3 million patient records across 14 different drug classes. They compared outcomes like hospitalizations, emergency room visits, and treatment failure rates. The results? For 12 out of 16 comparisons, there was no statistically significant difference between generic and brand-name drugs. For example:- Generic amlodipine led to 9% fewer heart attacks and strokes than the brand version.
- Generic glipizide had the same rate of insulin initiation as the brand - meaning both controlled blood sugar equally well.
- Generic quinapril showed no difference in hospitalizations for heart-related events.
The Psychiatric Drug Misconception
You’ve probably heard the claim: "Generics don’t work for depression or anxiety." That idea comes from a few studies that showed slightly higher psychiatric hospitalization rates with generics. But dig deeper. The same PLOS Medicine study found that patients on generic escitalopram or sertraline had a 5-7% higher chance of hospitalization. At first glance, that sounds alarming. But here’s the catch: when researchers compared authorized generics (made by the brand-name company) to the original brand, they saw the same pattern. That means the difference isn’t about the drug - it’s about perception. Patients who switch from a brand they recognize to a generic they don’t - even if it’s identical - sometimes feel like something’s wrong. They report side effects that aren’t there. They worry. And that anxiety can affect how they feel. The drug isn’t failing. The belief is. The FDA’s 2017 review of over 12 drug products found no consistent increase in patients switching back to brand-name drugs after starting a generic. That’s proof: when patients are educated, they stay on generics without issue.Why Some Providers Still Doubt
Let’s be honest - some hesitation is rooted in experience, not evidence. A few providers remember a patient who said, "This generic doesn’t work like the other one." Maybe the pill looked different. Maybe the patient had a bad experience years ago. Or maybe the pharmacy switched brands mid-prescription, and the patient noticed a change in size, color, or coating. But here’s what the data says: those differences in appearance - caused by inactive ingredients like dyes or fillers - have no impact on how the drug works. A 2019 FDA study confirmed this. The active ingredient is the same. The absorption is the same. The outcome is the same. The bigger issue? Cost. Generics are 80-85% cheaper. That’s why 90% of all prescriptions in the U.S. are filled with generics. The Congressional Budget Office estimates generics saved the healthcare system $1.68 trillion between 2008 and 2017. If you’re not prescribing generics, you’re not just missing out on cost savings - you’re potentially denying patients access to consistent, life-saving care.What You Need to Know About the Orange Book
The FDA’s Orange Book is your go-to tool for evaluating therapeutic equivalence. It rates generics as either "A" (therapeutically equivalent) or "B" (not equivalent). Over 97% of generics are rated "A." That means you can prescribe them with confidence. The 3% that are "B-rated"? These are complex products - like inhalers, topical creams, or injectables - where bioequivalence is harder to prove. For these, check the specific product labeling. If a generic is "B-rated," it’s not because it’s unsafe. It’s because the science is still evolving. But even then, most "B-rated" products still work fine for most patients.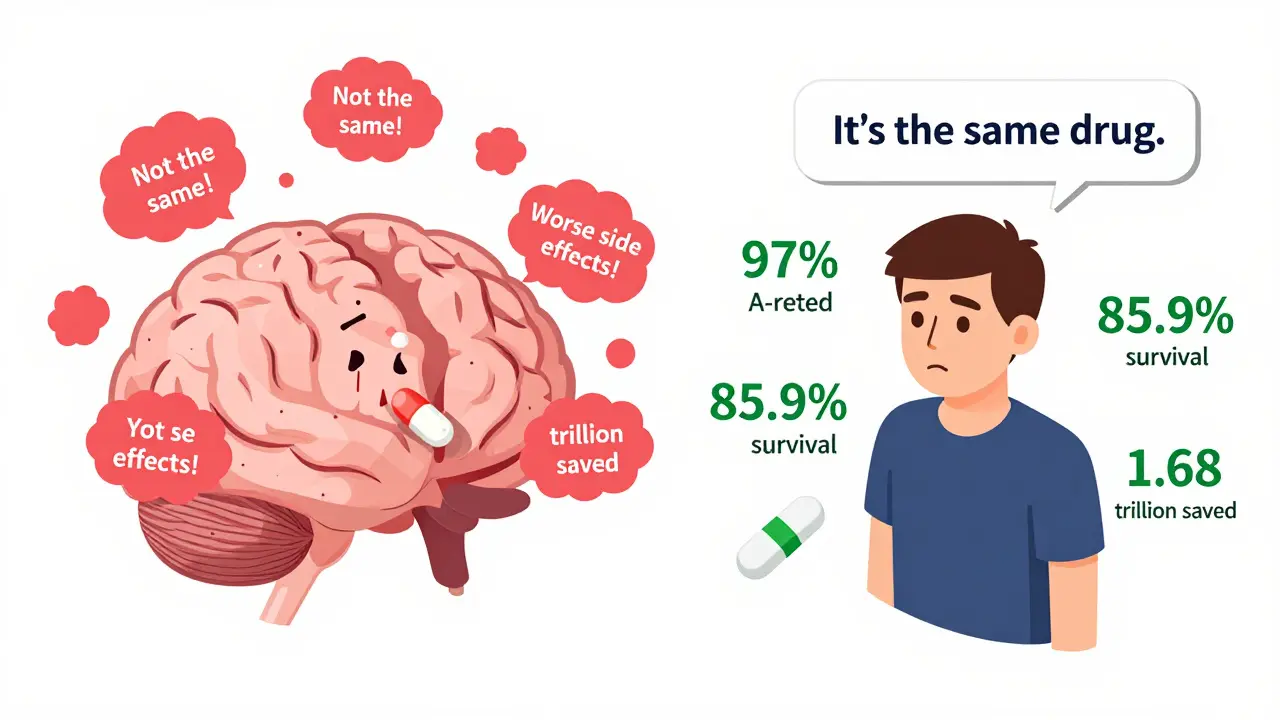
How to Talk to Patients
The biggest barrier to generic use isn’t science. It’s communication. Patients don’t trust what they don’t understand. If you say, "It’s the same thing," they’ll think you’re cutting corners. But if you say, "This generic has been tested in over 30 clinical studies and meets the same FDA standards as the brand - and it’s saved you $120 this month," that’s different. Use simple analogies: "It’s like buying store-brand aspirin. The active ingredient is identical. The packaging is different. The effect? The same." And if a patient insists on the brand? Ask why. Is it cost? Fear? Past experience? Address it. Offer to check if an authorized generic is available. Or suggest a trial period. Most patients who try a generic and see no difference stick with it.What the Numbers Don’t Lie About
A 2020 study of 3.5 million Medicare beneficiaries looked at five-year survival rates. At first glance, generic users had a higher survival rate - 85.9% vs. 77.8%. That sounds like generics are better. But when researchers adjusted for health status - because healthier people are more likely to get generics - the gap closed. The real difference? Not in the drug. In the patient. That’s the pattern across every major study: generics don’t outperform brands. They perform the same. And because they’re cheaper, more people take them consistently. That’s where the real benefit lies.What’s Next?
The FDA is updating its standards for complex generics - things like biosimilars and inhalers. But the core principle hasn’t changed: if a generic is approved, it’s as safe and effective as the brand. In 2022, the FDA approved 1,127 new generic drugs. That’s more than three per day. And with over 13,000 generics on the market, there’s rarely a reason not to prescribe one. The American College of Physicians says it plainly: "Physicians should generally prescribe generic drugs rather than brand-name drugs when equivalent generics are available." You don’t need to guess. You don’t need to worry. The data is there. The evidence is overwhelming. Generics work. And for your patients - and the healthcare system - that’s not just good news. It’s essential.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same strict manufacturing and quality standards as brand-name drugs. The active ingredient is identical, and the drug must be absorbed at the same rate and to the same extent. Adverse event reports show only 0.02% of all drug-related safety issues involve generics - far lower than the rate for brand-name drugs.
Why do some patients say generics don’t work for them?
Often, it’s not the drug - it’s the change. Switching from a familiar brand to a different-looking generic can trigger psychological concerns. Patients may notice a different pill shape, color, or taste and assume something’s wrong. In rare cases, inactive ingredients (like dyes or fillers) cause minor reactions, but these are not related to the drug’s effectiveness. Studies show that once patients are educated and given time to adjust, their concerns fade.
Can I switch a patient from a brand-name drug to a generic without risk?
For the vast majority of drugs - over 97% - yes. The FDA classifies these as "A-rated," meaning they are therapeutically equivalent. Even for drugs with narrow therapeutic indexes, like levothyroxine or warfarin, multiple studies show no clinically significant difference in outcomes when switching. The key is monitoring the patient briefly after the switch and ensuring they understand the change is routine, not a compromise.
Do generics take longer to work than brand-name drugs?
No. Bioequivalence testing requires generics to reach the same peak concentration in the bloodstream at the same time as the brand-name drug. If a generic took longer to work, it would fail FDA approval. Studies measuring absorption rates confirm this - there is no meaningful delay in onset for approved generics.
Why are generics so much cheaper if they’re the same?
Brand-name drugs carry the cost of research, development, marketing, and patent protection - which can exceed $2 billion per drug. Generics don’t repeat those costs. They only need to prove they match the existing drug. Once the patent expires, multiple manufacturers can produce the drug, driving prices down through competition. That’s why generics cost 80-85% less - not because they’re inferior, but because they’re more efficient.
Should I avoid prescribing generics for elderly patients?
No. In fact, elderly patients benefit the most. They’re more likely to struggle with high drug costs and skip doses. Generics improve adherence, reduce financial strain, and maintain clinical outcomes. Studies in Medicare populations show no increase in adverse events or hospitalizations when switching to generics. The American College of Physicians specifically recommends generics for older adults to improve access and compliance.
