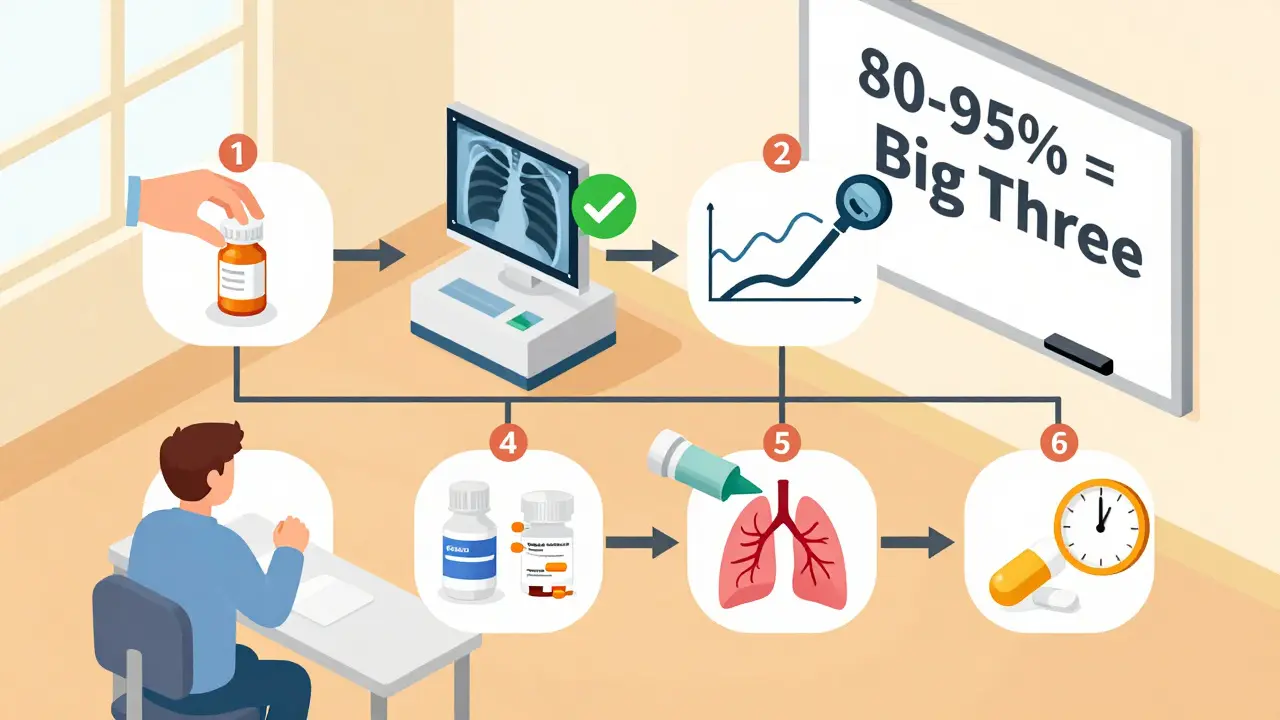
If you’ve been coughing for more than two months and no one can tell you why, you’re not alone. About 1 in 10 adults deal with a chronic cough - and most of them are told it’s "just allergies" or "stress" before anyone checks the real causes. The truth? In 80 to 95% of cases, it’s one of three things: GERD, asthma, or postnasal drip (now called upper airway cough syndrome). But here’s the catch: you can’t guess which one. You need a smart, step-by-step workup - or you’ll waste months on the wrong meds.
What Counts as a Chronic Cough?
A cough that lasts longer than eight weeks is considered chronic. That’s not a typo. It’s not a cold that won’t quit. It’s not a lingering flu. If your cough has dragged on past two months, especially if it’s dry, worse at night, or triggered by eating or lying down, it’s time to look beyond the obvious. Most people assume it’s a lung infection or bronchitis. But in nonsmokers not taking ACE inhibitors (blood pressure meds like lisinopril), those are rare. The real culprits are hidden - in your throat, your stomach, or your airways.
First Step: Rule Out the Dangerous Stuff
Before you chase GERD or allergies, you need to make sure it’s not something serious. A chest X-ray is the first test every doctor should order. It rules out pneumonia, lung cancer, tuberculosis, or scarring from past infections. If your X-ray looks normal - which it does in 90% of chronic cough cases - you’re not out of the woods, but you’re in the right lane.
Also, check your meds. If you’re on an ACE inhibitor - common for high blood pressure - that cough might be a side effect. It can start anytime between a week and six months after you begin the drug. Stopping it often clears the cough in days. No need for fancy tests. Just switch to a different pill.
Red flags? Coughing up blood, unexplained weight loss, fever that won’t break, or wheezing you’ve never had before. These mean you need more than a basic workup. Get referred to a pulmonologist fast.
The Big Three: GERD, Asthma, and Upper Airway Cough Syndrome
These three cause nearly all chronic coughs in adults who don’t smoke or take ACE inhibitors. The trick is, they don’t always act like you’d expect.
1. Asthma - Especially Cough Variant Asthma
Most people think asthma means wheezing and shortness of breath. But in about 25% of chronic cough cases, cough is the only symptom. That’s called cough variant asthma. You might feel fine otherwise. No chest tightness. No wheeze. Just a persistent, tickly cough - often worse at night or after exercise.
How do you test for it? Spirometry. It’s a simple breathing test. If your lung function looks normal, the next step is a methacholine challenge. This isn’t scary - you inhale a mist that slightly irritates your airways. If your lungs react with a 12% drop in airflow, you’ve got asthma. Even if your spirometry is normal, a positive methacholine test confirms it.
And here’s the good news: if it’s asthma, you’ll usually feel better within two to four weeks of starting an inhaled steroid. No need for antibiotics. No surgery. Just a puff or two a day.
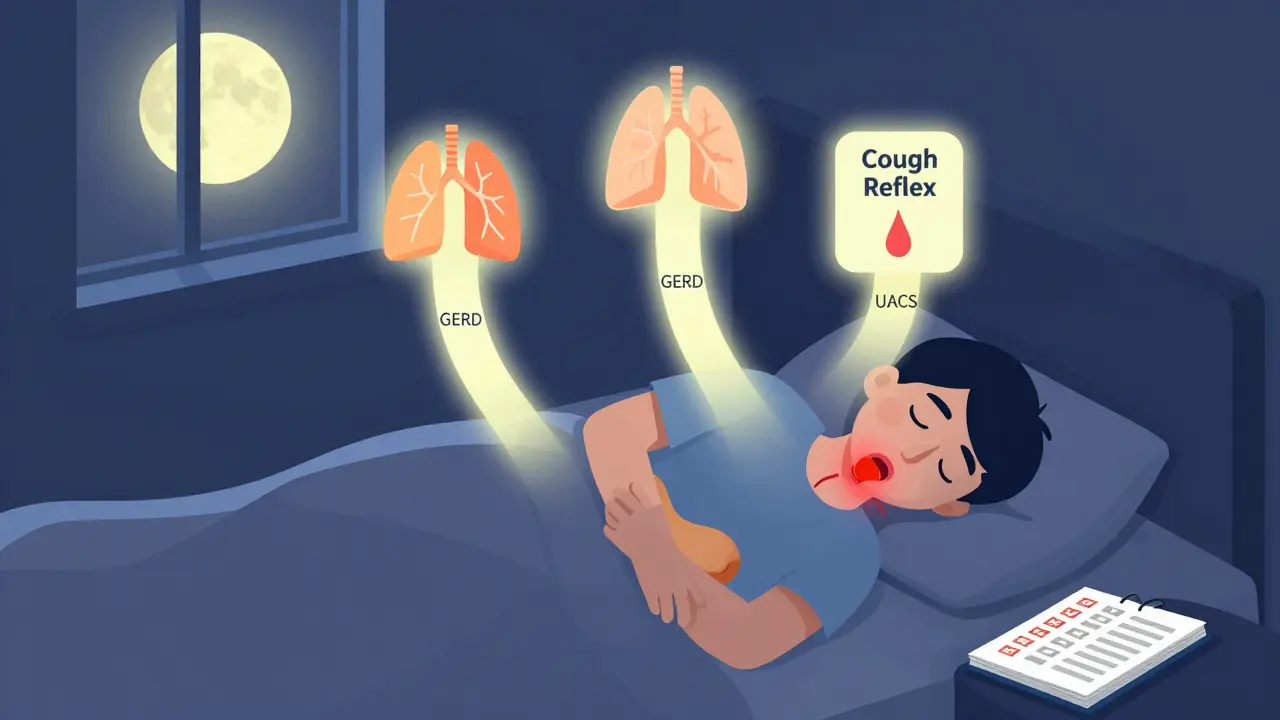
2. GERD - The Silent Culprit
GERD means stomach acid backs up into your esophagus. Classic symptoms? Heartburn, sour taste, bloating. But here’s the twist: up to 70% of people with GERD-related cough have no heartburn at all. It’s called silent reflux. The acid doesn’t burn your chest - it irritates your throat and triggers your cough reflex.
Diagnosing it is messy. A 24-hour pH monitor can detect acid in your esophagus, but it only catches abnormalities in 50-70% of cases. Blood tests? Useless. Endoscopy? Often normal. So the standard test is a therapeutic trial: take a high-dose proton pump inhibitor (PPI) like omeprazole twice a day for four to eight weeks.
Only half to three-quarters of people respond. That’s why doctors don’t just prescribe PPIs blindly anymore. The American College of Gastroenterology updated its guidelines in March 2024 to say: don’t start PPIs without first ruling out asthma and postnasal drip. And even then, if you don’t improve after eight weeks, it’s probably not GERD.
3. Postnasal Drip (Upper Airway Cough Syndrome)
This one’s the most common - responsible for up to 62% of chronic cough cases. But the name is misleading. It’s not just mucus dripping down your throat. It’s inflammation in your nasal passages and sinuses that makes your cough reflex hypersensitive. That’s why it’s now called upper airway cough syndrome (UACS).
Think: allergies, colds, sinus infections. You might have a runny nose, itchy eyes, or feel like you’re clearing your throat all day. But sometimes, there’s no obvious nasal symptom. Just the cough.
Here’s how you test it: take a first-generation antihistamine (like brompheniramine) with a decongestant (like pseudoephedrine) for two to three weeks. No nasal sprays. No second-gen antihistamines like loratadine - they don’t work as well for this. If your cough improves by 70-90%, you’ve got UACS. Response usually comes within days, not weeks.
How Doctors Decide the Order
Not all doctors follow the same sequence. But the best approach - backed by the American College of Chest Physicians - is to test for UACS and asthma first. Why? Because they respond faster and more reliably to treatment.
Start with:
- Rule out ACE inhibitors and red flags
- Do a chest X-ray
- Do spirometry
- Trial for UACS (antihistamine + decongestant) for 2 weeks
- If no improvement, trial for asthma (inhaled steroid) for 4 weeks
- If still no improvement, trial for GERD (PPI) for 8 weeks
That’s it. No CT scans. No blood work. No swallowing studies. Unless you’re not improving after this, you’re not wasting time or money.
Why This Works Better Than Guessing
Many patients get stuck in a loop: antibiotics for a "bacterial cough," then cough suppressants, then herbal teas, then chiropractic adjustments. None of those fix the root cause.
Here’s what happens when you skip the workup:
- You take PPIs for months - and they don’t help - because it’s not GERD.
- You use nasal sprays - but they’re for congestion, not cough reflex sensitivity.
- You get a CT scan - and it’s normal - but you paid $1,000 and got radiation equal to 74 chest X-rays.
With the right workup, most people feel better in 4 to 8 weeks. Not 6 months. Not a year.
What If Nothing Works?
About 10-30% of chronic cough cases don’t respond to the big three. That’s when you dig deeper. Possible causes:
- Chronic refractory cough (CRC) - your cough reflex is just too sensitive
- Pertussis (whooping cough) - rare in adults, but possible if you haven’t had a booster
- Chronic aspiration - swallowing problems that send food into your lungs
- Eosinophilic bronchitis - inflammation without asthma
New tools are emerging. The Hull Cough Questionnaire scores how much your cough affects your life. A score above 15 means severe impact. The Hull Airway Reflux Questionnaire (HARQ) helps spot silent reflux - a score over 13 suggests laryngopharyngeal reflux with 80% accuracy.
And there’s new medicine. Gefapixant, approved in late 2022, reduces cough frequency by 18-22% in people with CRC. Camlipixant, under FDA review as of May 2024, showed even better results in trials. These aren’t cures, but they’re the first drugs designed specifically for chronic cough.
What You Can Do Today
You don’t need to wait for a specialist. Here’s your action plan:
- Stop any ACE inhibitor if you’re on one - talk to your doctor first.
- Get a chest X-ray if you haven’t had one in the last 6 months.
- Try a 2-week trial of brompheniramine + pseudoephedrine (check with your pharmacist - some need a prescription).
- If no change, start an inhaled steroid (like fluticasone) for 4 weeks.
- If still no improvement, try omeprazole 20mg twice daily for 8 weeks.
- Keep a cough diary: when it happens, what triggers it, how bad it is.
Don’t just endure it. Track it. That’s how you give your doctor the clues they need.
What’s Changing in 2026
AI is starting to help. A 2023 study in Lancet Digital Health showed an algorithm could tell apart asthma cough from GERD cough just by analyzing the sound - 87% accuracy. It’s not in clinics yet, but it’s coming.
Terminology matters too. "Postnasal drip" is outdated. It’s not about mucus dripping - it’s about nerve sensitivity in your throat. That’s why the term "upper airway cough syndrome" is now standard.
And insurance? Still a mess. Many won’t cover pH monitoring unless you’ve tried everything else. But that’s changing. With new drugs approved, payers are starting to fund better testing.
The bottom line? Chronic cough isn’t a mystery anymore. It’s a solvable puzzle. And you don’t need to be a doctor to start solving it - just patient, persistent, and ready to follow the steps.
Can a chronic cough be caused by something I ate?
Yes - but not because of the food itself. If you have GERD, certain foods like spicy meals, chocolate, coffee, or large dinners can trigger acid reflux, which then irritates your throat and causes coughing. But if you don’t have reflux, changing your diet won’t help. The issue isn’t the food - it’s whether your stomach acid is moving up into your throat.
Why do I cough more at night?
Nighttime coughing is a classic sign of either asthma or GERD. When you lie down, stomach acid flows more easily into the esophagus, triggering reflux. Also, airways naturally narrow at night - which makes asthma symptoms worse. Postnasal drip can also worsen at night if you’re breathing through your mouth due to nasal congestion.
Do I need a CT scan for my chronic cough?
No - not unless your chest X-ray is abnormal or you have red flags like weight loss or coughing up blood. A normal X-ray means serious lung disease is extremely unlikely. A CT scan exposes you to high radiation (equivalent to 74 chest X-rays) and rarely finds anything new. Guidelines strongly advise against it unless absolutely necessary.
Can allergies cause chronic cough?
Allergies themselves don’t directly cause coughing - but they can trigger upper airway cough syndrome. When your nasal passages swell from allergens, mucus builds up and irritates your throat, making your cough reflex oversensitive. That’s why antihistamines help - not because they treat allergies, but because they calm the nerve signals causing the cough.
Is it safe to take OTC cough medicine for chronic cough?
Most over-the-counter cough syrups - like dextromethorphan - don’t work for chronic cough. They suppress the cough reflex temporarily, but they don’t fix the underlying cause. In fact, they can mask symptoms and delay real treatment. For chronic cough, targeted therapy for GERD, asthma, or UACS is far more effective than any cough drop.
How long should I wait before seeing a specialist?
If you’ve tried the three-step workup - UACS trial, asthma trial, GERD trial - and still have no improvement after 12 weeks, it’s time to see a pulmonologist or ear, nose, and throat specialist. Don’t wait longer than that. Persistent cough beyond three months can lead to vocal cord damage, rib fractures, or sleep deprivation - and newer treatments like gefapixant are now available for those who don’t respond to standard care.
Chronic cough isn’t something you live with. It’s something you fix - with the right steps, the right timing, and the right mindset. Start with the basics. Track your symptoms. Don’t settle for "it’s just a cough." Your lungs deserve better.
