When you’re on treatment for osteoporosis, waiting a year or two to see if your bones are getting stronger can feel like guessing in the dark. That’s where bone turnover markers come in-they give you real-time feedback on whether your medication is working, long before a scan can show any change.
What Are Bone Turnover Markers?
Bone isn’t static. It’s constantly being broken down and rebuilt in a process called remodeling. When bone breaks down, fragments of collagen and other proteins spill into your blood and urine. These are bone turnover markers (BTMs). When new bone forms, different proteins show up. By measuring these, doctors get a snapshot of how active your bone remodeling is right now.
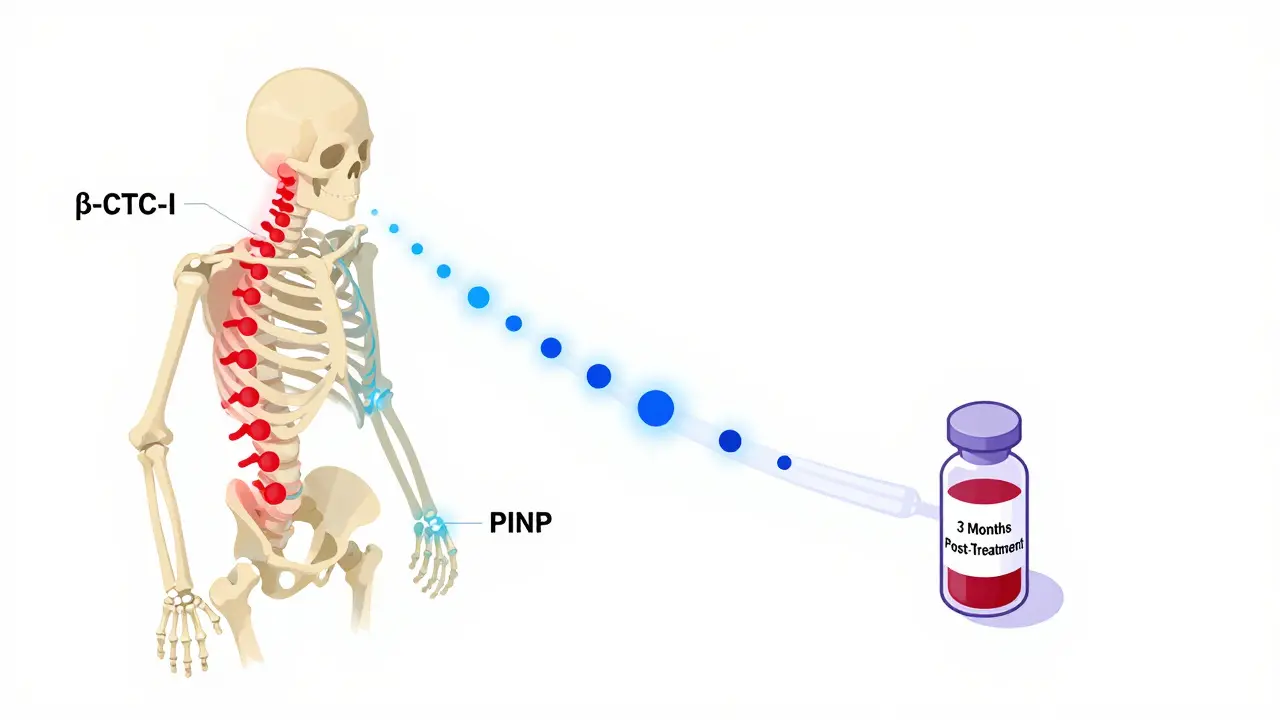
There are two types: resorption markers (signs of bone breakdown) and formation markers (signs of bone building). The two most trusted markers today are serum PINP (procollagen type I N propeptide) and plasma β-CTX-I (beta-C-terminal telopeptide of type I collagen). PINP tells you how fast new bone is being made. β-CTX-I shows how fast old bone is being removed.
Why these two? Because they’re the most stable, accurate, and well-studied. Other markers like osteocalcin or urinary NTx exist, but they’re more affected by things like food, time of day, or kidney function. PINP and β-CTX-I have been standardized across labs worldwide, making results easier to compare.
Why Use Them Instead of Just a Bone Scan?
Dual-energy X-ray absorptiometry (DXA) scans measure bone mineral density-the gold standard for diagnosing osteoporosis. But here’s the catch: it takes 12 to 24 months to see a meaningful change in bone density after starting treatment. That’s a long time to wonder if your pills are working.
Bone turnover markers change much faster. Within 3 to 6 weeks of starting an anti-resorptive drug like a bisphosphonate, you’ll see a drop in β-CTX-I. By 3 months, that drop is clear. A reduction of more than 30% in β-CTX-I or 35% in PINP means your body is responding. If you’re on an anabolic drug like teriparatide, PINP will spike-sometimes by 70% to 100%-showing your bones are building new tissue.
Think of it like checking your car’s engine light. A DXA scan tells you how far you’ve driven. BTMs tell you if the engine is running properly right now.
How Are They Used in Real Treatment?
Here’s how it works in practice:
- Before you start treatment, your doctor takes a baseline blood test for PINP and β-CTX-I.
- After 3 months on medication, you get tested again.
- If β-CTX-I dropped by more than 30%, or PINP dropped by more than 35%, you’re responding well.
- If not, your doctor looks at why: Did you miss doses? Is your kidney function affecting the results? Is another condition interfering?
This isn’t just about checking if the drug works-it’s about catching non-adherence early. Studies show BTM monitoring identifies patients who aren’t taking their meds with 85% accuracy. That’s huge. Many people stop osteoporosis drugs because they don’t feel immediate results. But if you know your marker levels are dropping, you’re more likely to stick with it.
For patients with chronic kidney disease, things get trickier. Kidneys clear these markers. When they’re not working well, PINP and β-CTX-I can build up even if bone turnover is normal. In these cases, doctors may use bone alkaline phosphatase (BALP) or TRACP5b instead-markers less affected by kidney function.

Getting Accurate Results: The Fine Print
These tests are powerful, but only if done right. A single mistake can throw off the result.
For β-CTX-I, you must fast overnight. Eat anything, and your levels can jump 20-30%. You also have to have the blood drawn between 8 and 10 a.m. because CTX levels rise and fall with your body clock-up to 40% variation in a single day. PINP is more stable, but still best measured in the morning.
Even the lab matters. Not all labs follow the same protocols. The International Osteoporosis Foundation and European Calcified Tissue Society recommend specific methods and reference ranges. In the U.S., only about 65% of labs meet these standards. Ask your doctor: Do you use IFCC-recommended assays for PINP and β-CTX-I?
And don’t forget: BTMs reflect your whole skeleton. They don’t tell you if your hip or spine is improving specifically. That’s still the job of the DXA scan. BTMs are the early warning system. DXA is the final report.
Who Benefits Most From This?
Bone turnover markers aren’t for everyone. They’re most useful in three situations:
- People starting anti-resorptive therapy (like alendronate or denosumab) who need early confirmation it’s working.
- People on anabolic drugs (like teriparatide or romosozumab) where a strong PINP rise confirms the drug is activating bone building.
- Patients with poor adherence or suspected non-compliance-especially if their DXA results don’t improve as expected.
They’re less useful for routine follow-up in people who are doing fine. If you’ve been on treatment for two years and your DXA is stable, you probably don’t need BTMs every year.
Also, they’re not used for diagnosis. Osteoporosis is diagnosed by DXA scan, not by marker levels. BTMs help you manage what’s already diagnosed.
What’s Changing in 2026?
Guidelines are evolving. In 2023, major organizations like the International Osteoporosis Foundation and the European Society for Clinical and Economic Aspects of Osteoporosis officially endorsed PINP and β-CTX-I as the reference markers. That’s a big deal-it means more doctors are starting to use them.
Insurance coverage is improving too. Medicare in the U.S. has covered these tests since 2020. Reimbursement is modest-around $30 per test-but it’s there. In Europe, 45-60% of clinics now use BTMs regularly. In the U.S., adoption is still around 25-35%, but rising.
Research is expanding. Clinical trials are now testing whether using BTMs to adjust treatment-like switching drugs early if there’s no response-can reduce fractures more than waiting for DXA results. Early data looks promising.
One big gap: most reference ranges are based on Caucasian populations. Asian patients often have lower baseline CTX levels. African populations tend to have higher PINP. Labs are starting to adjust for this, but it’s not universal yet.
What to Ask Your Doctor
If you’re on osteoporosis treatment, here’s what to bring up:
- Can we check my PINP and β-CTX-I before I start treatment?
- When should I get tested again? Is 3 months the right time?
- Do you use the IFCC-recommended assays for these markers?
- What’s my target reduction? Should my β-CTX-I drop by 30% or more?
- What if my numbers don’t change? What are the next steps?
These questions show you’re engaged-and they help your doctor give you better care.
The Bottom Line
Bone turnover markers aren’t magic. They won’t replace DXA scans. But they give you something no scan can: early, objective proof that your treatment is working. For someone worried about fractures, that’s powerful. For someone struggling to stick with daily pills, it’s motivation. For a doctor trying to personalize care, it’s a tool.
The science is solid. The guidelines are clear. The technology is available. The only thing holding it back is awareness-and that’s changing fast. If you’re on osteoporosis therapy, ask about BTMs. You might be surprised how much they can tell you-long before your next bone scan.