When you hear the word generic, you probably think of cheap pills that work just like the brand-name ones. And for small-molecule drugs, that’s true. But when it comes to biologics-complex medicines made from living cells-things get much more complicated. Enter biosimilars. They’re not generics. They’re not copies. And confusing them can lead to real misunderstandings about cost, safety, and how your treatment works.
What Are Generics, Really?
Generics are the workhorses of modern medicine. They’re small-molecule drugs made from chemicals, not living cells. Think ibuprofen, metformin, or amoxicillin. Once the patent on a brand-name drug expires, other companies can make the exact same chemical compound. The FDA requires them to be bioequivalent: meaning they absorb into your bloodstream at the same rate and to the same extent as the original. That’s it. No need for massive clinical trials. Just proof that your body handles it the same way. Because the chemistry is simple and repeatable, generics cost 40% to 50% less than the brand versions. Over 90% of prescriptions in the U.S. are filled with generics. They’re everywhere-pharmacies, hospitals, mail-order services. And because they’re chemically identical, pharmacists can swap them in automatically without asking your doctor. In fact, in every state, you’re likely getting a generic unless you specifically ask for the brand.What Are Biosimilars?
Biosimilars are the cousins of generics, but they’re not twins. They’re made from living organisms-usually cells grown in labs. These are large, complex proteins like monoclonal antibodies. Examples include drugs for rheumatoid arthritis (like adalimumab), cancer (like trastuzumab), and diabetes (insulin). Because they come from living systems, no two batches are perfectly identical. Even the original manufacturer can’t make the exact same molecule twice. That’s just how biology works. A biosimilar isn’t supposed to be identical to the original biologic. It just has to be highly similar with no clinically meaningful differences in safety, purity, or effectiveness. The FDA requires hundreds of tests-analyzing structure, function, immune response, and sometimes small clinical studies-to prove that. It’s not a shortcut. It’s a longer, more expensive road. Developing a biosimilar costs $100 million to $200 million. For a generic? Around $2 million to $5 million.Why the Big Price Difference?
Generics drop prices hard because they’re easy to copy. Biosimilars? They’re hard to copy. Even if you know the target protein, you don’t know the exact cell line, fermentation process, purification steps, or storage conditions the original company used. Those are trade secrets. So biosimilar makers have to reverse-engineer the whole thing from scratch. That’s why biosimilars only save 15% to 33% compared to the original biologic-not the 50% you get with generics. The cost of development, testing, and manufacturing is just too high. And even though they’re cheaper than the brand, they’re still expensive. A single dose of a biosimilar for cancer or autoimmune disease can still cost thousands.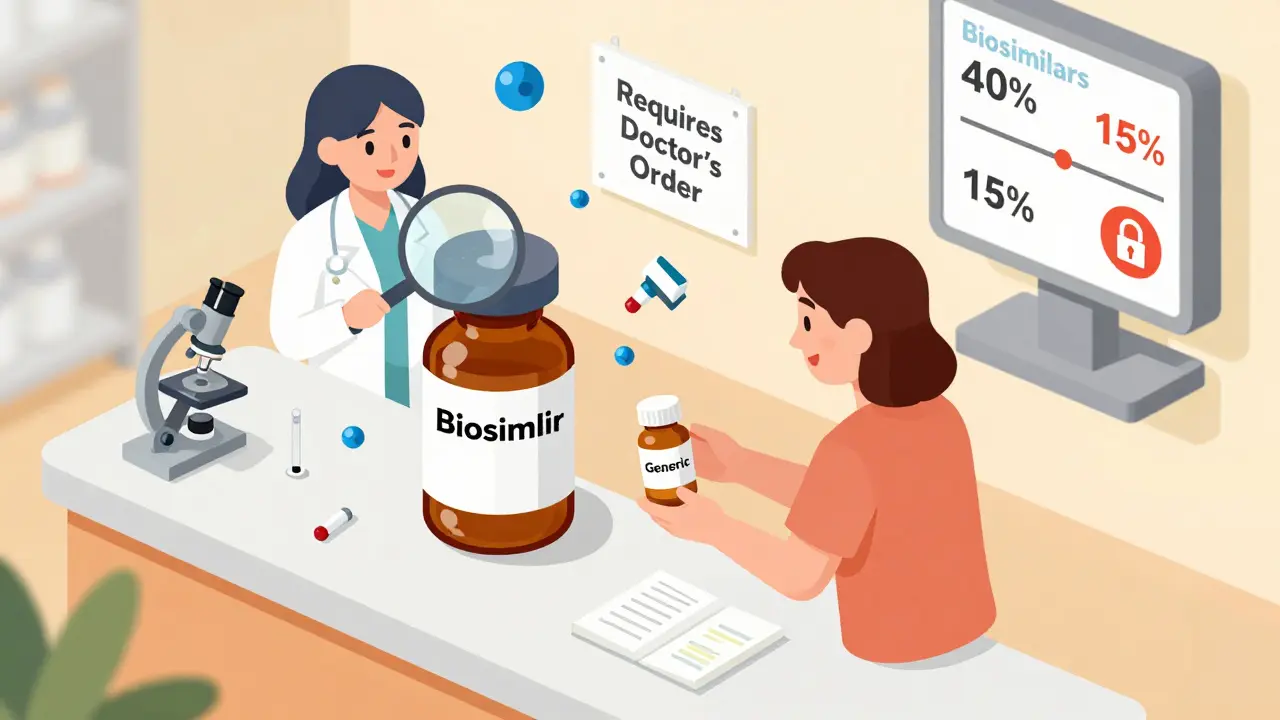
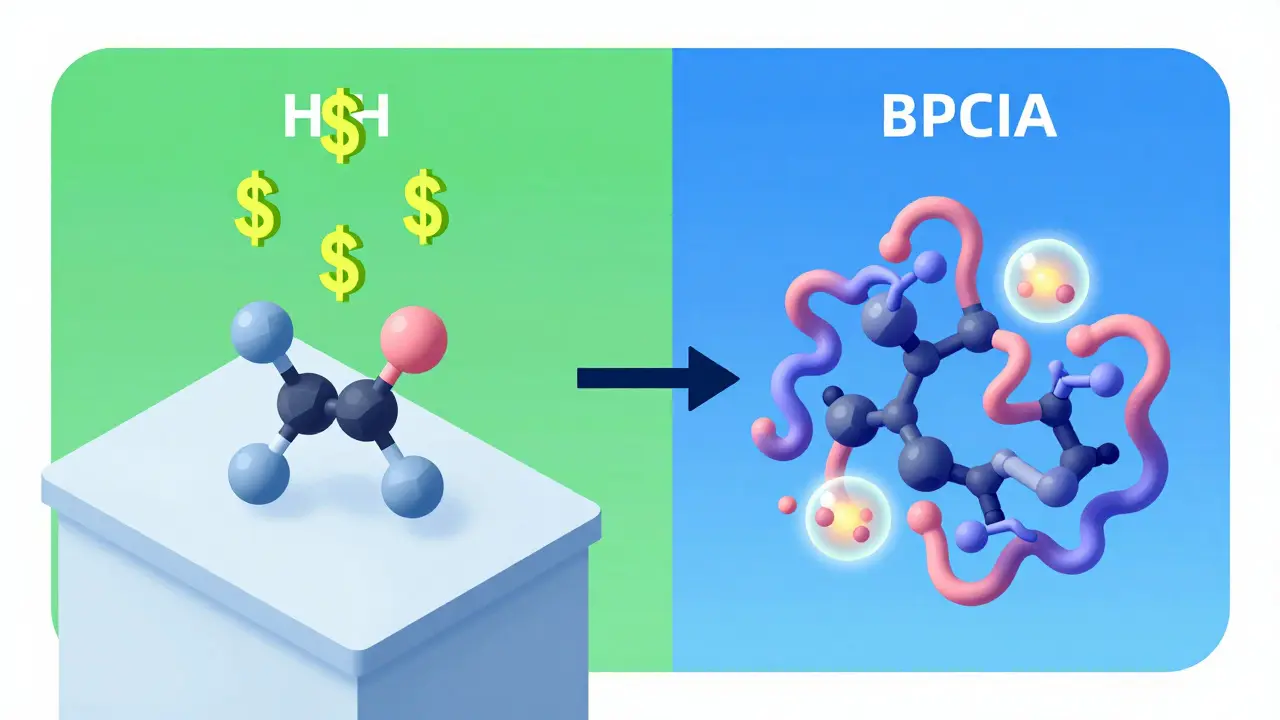
Regulatory Pathways: Two Different Rules
The FDA handles generics and biosimilars under two completely different laws. Generics follow the Hatch-Waxman Act of 1984. Biosimilars follow the Biologics Price Competition and Innovation Act (BPCIA) of 2009. That’s why the approval processes are so different. For generics: prove bioequivalence. That usually means testing blood levels in 20 to 50 healthy volunteers. Done in months. For biosimilars: prove similarity through analytical testing, animal studies, pharmacokinetic data, and sometimes clinical trials in hundreds of patients. It takes years. And you can’t skip steps. The FDA won’t approve a biosimilar unless it matches the reference product across dozens of quality attributes.Can You Swap Them Like Generics?
This is where things get tricky. In every state, pharmacists can swap a generic for a brand-name drug without telling you or your doctor. It’s automatic. But with biosimilars? Not so fast. Only biosimilars that are designated as “interchangeable” can be swapped automatically. And as of late 2023, only seven out of 42 approved biosimilars have that status. The rest? Your doctor has to specifically prescribe them. If you’re on a biologic and your insurance wants to switch you to a biosimilar, you’ll likely need prior authorization-and maybe even a new prescription. Why the hesitation? Because biologics can trigger immune reactions. If you’ve been stable on a drug for years, switching to a biosimilar-even one proven safe-can raise concerns about flare-ups or side effects. Many rheumatologists and oncologists prefer to stay on the original unless there’s a strong financial incentive or clear clinical reason to switch.Market Reality: Generics Dominate, Biosimilars Are Growing
Generics make up 90% of all prescriptions filled in the U.S., but only 20% of total drug spending. That’s because they’re cheap. Biosimilars? They’re under 3% of the biologics market-even though biologics account for nearly half of all U.S. drug spending. That’s the disconnect. Biologics are expensive, and biosimilars could save billions… but adoption is slow. Why? Several reasons. First, the original manufacturers fight hard. AbbVie, for example, filed over 240 patents on Humira to delay competition. Second, reimbursement systems like “buy and bill” in hospitals make it financially easier for providers to stick with the brand. Third, many patients and doctors are just unfamiliar with biosimilars. A 2022 survey found 68% of rheumatologists wanted more education before prescribing them. But things are changing. In early 2024, the first interchangeable biosimilar for Humira hit the market with a 35% price cut. More are coming. By 2028, analysts expect biosimilars to make up 25% to 30% of the U.S. biologics market. The Inflation Reduction Act is helping by capping insulin costs and closing Medicare Part D coverage gaps-making biosimilars more attractive to insurers and patients alike.
What This Means for You
If you’re taking a small-molecule drug-like a statin, blood pressure pill, or antibiotic-you’re almost certainly on a generic. No need to worry. It’s the same medicine, cheaper. But if you’re on a biologic-for Crohn’s disease, psoriasis, rheumatoid arthritis, or cancer-you might be offered a biosimilar. Ask your doctor: Is this a biosimilar? Is it interchangeable? What’s the evidence behind switching? Will my insurance cover it? Will I need to be monitored differently? Don’t assume biosimilars are riskier. They’re not. The FDA’s standards are strict. But do understand they’re not the same as generics. They’re a different kind of medicine. And that matters.Common Myths, Cleared Up
- Myth: Biosimilars are just generic biologics. Truth: They’re not. Biologics are too complex to be copied exactly. Biosimilars are highly similar, not identical.
- Myth: Switching to a biosimilar is unsafe. Truth: For most patients, it’s safe. But it should be done thoughtfully, especially if you’re stable on the original.
- Myth: Biosimilars don’t save money. Truth: They do-15% to 35%-and that adds up fast when you’re treating chronic conditions in thousands of patients.
- Myth: Only Europe uses biosimilars. Truth: Europe adopted them faster, but the U.S. is catching up fast, especially with new interchangeable products.
Where to Find More Info
The FDA’s Purple Book lists all approved biologics and biosimilars, including which ones are interchangeable. It’s not as user-friendly as the Orange Book (which lists generics), but it’s the official source. The Biosimilars Forum and the American Society of Health-System Pharmacists also offer clear guides for patients and providers. If you’re confused about what you’re taking-ask. Your pharmacist can tell you if your drug is a biosimilar. Your doctor can explain why it was chosen. And your insurer can tell you if a switch is planned. The bottom line: biosimilars are not generics. But they’re not scary, either. They’re a necessary step toward making life-changing medicines more affordable. Understanding the difference helps you make smarter choices-and speak up when it matters.Are biosimilars the same as generics?
No. Generics are chemically identical copies of small-molecule drugs. Biosimilars are highly similar but not identical copies of complex biologic drugs made from living cells. They’re not interchangeable in terms of manufacturing or regulatory approval.
Can pharmacists substitute biosimilars like generics?
Only if the biosimilar has been designated as "interchangeable" by the FDA. As of late 2023, only 7 out of 42 approved biosimilars have that status. Most biosimilars require a specific prescription from your doctor. Generics, on the other hand, can be automatically substituted in all 50 states.
Why are biosimilars more expensive than generics?
Biosimilars cost $100 million to $200 million to develop because they’re made from living cells and require hundreds of tests to prove similarity. Generics cost $2 million to $5 million because they’re chemically identical and easier to replicate. The higher cost of development means biosimilars don’t drop in price as dramatically as generics do.
Are biosimilars safe?
Yes. The FDA requires biosimilars to show no clinically meaningful differences in safety, purity, or effectiveness compared to the original biologic. They undergo extensive testing, including studies on immune response. Thousands of patients have safely switched to biosimilars, especially in Europe where they’ve been used for over a decade.
Which conditions are treated with biosimilars?
Biosimilars are used for chronic and serious conditions like rheumatoid arthritis, Crohn’s disease, psoriasis, cancer (e.g., breast, colon), and diabetes. Common targets include drugs like Humira (adalimumab), Enbrel (etanercept), Remicade (infliximab), and Herceptin (trastuzumab). Generics, by contrast, cover nearly every common condition-from high blood pressure to infections.
Will my insurance force me to switch to a biosimilar?
It’s possible, especially if the biosimilar is cheaper and your plan covers it. But you should be notified first. If you’re stable on a biologic, your doctor can often request an exception. Always check with your insurer and ask your provider about any planned switches.