Why Patients Stick With Expensive Drugs Even When Cheaper Ones Work Just As Well
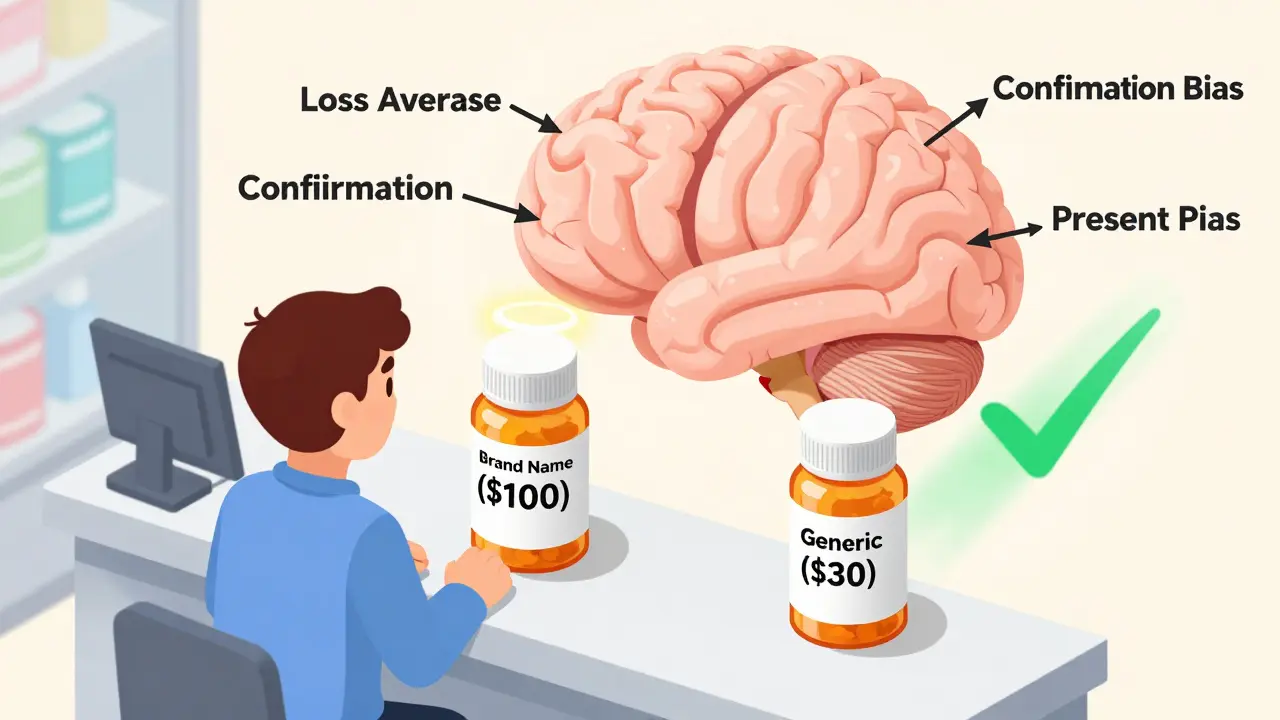
Imagine this: you’re prescribed a new medication. Your doctor says there’s a generic version that works just as well and costs 70% less. But you choose the brand-name drug anyway. Why? It’s not because you don’t care about money. It’s not because you’re misinformed. It’s because your brain isn’t wired to make purely logical choices when it comes to health.
This isn’t rare. In fact, it’s the norm. Behavioral economics explains why patients make drug choices that defy logic-and how we can use that knowledge to help them take their meds properly.
The Myth of the Rational Patient
For decades, healthcare systems assumed patients were rational actors. If a drug was cheaper and equally effective, they’d switch. Simple. But real people don’t work that way.
Studies show that 68% of patients stick with their current medication-even when a cheaper, equally effective alternative is available. Why? Fear. Loss aversion. Trust in the brand. These aren’t quirks. They’re predictable patterns.
Traditional education campaigns-handouts, pamphlets, YouTube videos-barely move the needle. Most improve adherence by only 5-8%. Behavioral economics, on the other hand, boosts adherence by 14-28%. That’s not a small win. That’s life-changing.
How Your Brain Tricks You Into Choosing the Wrong Drug
Your brain has shortcuts. They’re useful for deciding what to eat or which route to take to work. But when it comes to medication, they can be dangerous.
- Loss aversion: People feel the pain of losing something more intensely than the joy of gaining something equal. So if you’ve been on a drug for months, switching-even to something better-feels like a risk. You’re not choosing the drug. You’re avoiding the loss of what you’re used to.
- Confirmation bias: If you believe expensive = better, you’ll ignore evidence that a generic works just as well. A 2022 study found that patients who paid more for their meds reported fewer side effects-even when the pills were identical.
- Present bias: You know your blood pressure needs to be controlled. But right now? You’re tired. You forgot your pill. Tomorrow’s another day. That’s present bias. 33% of prescriptions are never even filled because the immediate hassle outweighs the distant benefit.
- Social norms: If you see other people taking a certain drug, you assume it’s the right one. One HIV clinic posted adherence rates on the wall. Within months, adherence jumped 22.3%. People didn’t want to be the one falling behind.
These aren’t flaws. They’re human. And when we ignore them, we set patients up to fail.
What Works: Real Nudges That Get People to Take Their Meds
Behavioral economics doesn’t force people. It makes the right choice easier.
Here’s what actually moves the needle:
- Defaults matter. In a 2012 hospital study, when pharmacists changed the default option in the electronic system from the brand-name drug to the generic, appropriate substitutions jumped 37.8%. No one had to ask. No one had to argue. It was just the standard.
- Framing changes everything. Telling patients a vaccine is “95% effective” leads to 18.4% more people getting it than saying it’s “5% ineffective.” The same fact, flipped. That’s the power of framing.
- Loss aversion in action. A 2021 study gave statin patients a $50 monthly rebate-unless they missed a dose. Those who could lose money took their pills 23.8% more often than those who got no incentive.
- Texts that trigger emotion. “Take your pill” gets ignored. “Don’t lose your streak!” triggers loss aversion and improved adherence by 19.7%.
These aren’t gimmicks. They’re science. And they’re being used by hospitals, insurers, and big pharma right now.

Why Some Patients Still Don’t Adhere-Even With Nudges
Not everyone responds the same way.
Patients with depression or anxiety see 31.4% less benefit from behavioral interventions. Why? Mental health conditions mess with decision-making circuits. A nudge won’t help if the brain’s ability to plan and follow through is impaired.
Other barriers are structural:
- Polypharmacy: Each extra pill you take cuts adherence by 8.3%. Ten pills? You’re likely skipping doses.
- Asymptomatic conditions: If you don’t feel sick, why take a pill? Adherence drops 32.7% for drugs treating high blood pressure or cholesterol.
- Negative beliefs: 41.2% of people stop their meds because they believe the drug is unnecessary, harmful, or just a “money grab.”
There’s no one-size-fits-all fix. But there is a smarter approach: match the nudge to the barrier.
What’s Changing in Healthcare-And Why It Matters
Behavioral economics is no longer just research. It’s policy.
The FDA’s 2023 guidance now requires drug makers to prove they’ve considered how dosing frequency and pill size affect patient decisions. That’s huge. It means companies can’t just design drugs for convenience-they have to design them for human behavior.
Medicare Part D now requires insurance plans to use at least two behavioral interventions for high-risk patients. That’s not optional. It’s mandatory.
Pharmaceutical companies are investing heavily. McKinsey found that firms using behavioral nudges in patient support programs saw 17.3% higher medication persistence and 22.8% fewer discontinuations.
And the market is booming. The global healthcare behavioral economics consulting market grew from $187 million in 2018 to $432 million in 2022. Big pharma, insurers, and hospitals are all in.
The Dark Side: When Nudges Become Manipulation
Not everyone is thrilled about this.
Some critics worry that nudging patients into certain drugs is unethical. Could insurers use loss aversion to push patients toward cheaper drugs-even if they’re not the best fit?
Dr. Aaron Kesselheim from Harvard says the key is preserving freedom. “You can nudge,” he says, “but you can’t force.” A well-designed nudge lets people opt out. It doesn’t trick them. It makes the right choice obvious.
That’s the line. Nudges that empower. Nudges that inform. Nudges that reduce friction-not pressure.
When done right, behavioral economics doesn’t take away choice. It makes better choices easier.

Where This Is Headed: AI, Personalization, and the Future of Adherence
The next wave? Personalized nudges.
Researchers are now using machine learning to predict who will respond to which nudge. One pilot study showed that by analyzing a patient’s age, income, mental health history, and past adherence, algorithms could predict their response to loss aversion, social norms, or defaults with 42.3% greater accuracy.
Smart pill bottles that text you when you miss a dose. Apps that show your “streak” of adherence. Insurance plans that reward consistent behavior with lower premiums.
These aren’t sci-fi. They’re rolling out now. And they’re working.
But the biggest win? It’s not just about taking pills. It’s about reducing hospitalizations, preventing deaths, and saving billions. Medication non-adherence costs the U.S. $289 billion a year and causes 125,000 avoidable deaths.
Behavioral economics isn’t about changing minds. It’s about changing systems. And that’s where real progress happens.
What You Can Do-Whether You’re a Patient or a Provider
If you’re a patient:
- Ask: “Is there a generic? Will it work the same?”
- Don’t assume price = quality.
- Use reminders-but make them emotional. “Don’t break your streak” works better than “Take your pill.”
If you’re a provider:
- Change your default prescriptions to the most effective, affordable option.
- Use framing. Say “This drug reduces your risk by 40%,” not “There’s a 60% chance it won’t help.”
- Track adherence-not just prescriptions filled, but doses taken.
If you’re a policymaker or insurer:
- Require behavioral interventions in formulary design.
- Invest in simple, low-cost tools: SMS reminders, default settings, rebate systems.
- Measure outcomes-not just cost savings, but hospital readmissions and mortality.
Final Thought: It’s Not About Willpower
People aren’t failing because they’re lazy or careless. They’re failing because the system doesn’t understand how they think.
Behavioral economics doesn’t blame the patient. It fixes the environment. And that’s the only way we’ll ever get adherence rates to climb.
The future of medicine isn’t just better drugs. It’s better design. Smarter choices. And systems that work with human nature-not against it.
Why do patients choose expensive drugs over cheaper generics?
Patients often choose expensive drugs due to psychological biases like loss aversion (fearing they’ll lose benefits of their current drug), confirmation bias (believing higher price means better quality), and trust in brand names. Studies show 68% of patients stick with their current medication-even when equally effective generics cost 30% less-because switching feels like a risk, not a savings.
How effective are behavioral nudges compared to patient education?
Behavioral nudges improve medication adherence by 14-28%, while traditional education programs typically improve adherence by only 5-8%. For example, using defaults in electronic prescribing systems increased appropriate generic substitutions by 37.8%, and loss aversion-based rebate programs boosted statin adherence by 23.8%. Nudges work because they change the environment, not just the information.
Can behavioral economics help with chronic conditions like diabetes or high blood pressure?
Yes. Diabetes has the highest adoption of behavioral interventions (47.8% of programs), because regular dosing creates clear opportunities for nudges. SMS reminders framed as “Don’t lose your streak!” improved adherence by 19.7%. Defaults in prescribing and loss aversion rebates also work well. For high blood pressure, where symptoms are absent, nudges that link daily habits to long-term outcomes are most effective.
Are behavioral nudges ethical?
They’re ethical when they preserve freedom of choice. A nudge makes the right option easier-not mandatory. For example, making a generic drug the default in a prescription system still lets doctors and patients choose the brand. Experts like Dr. Aaron Kesselheim argue that nudges respect autonomy while reducing harmful defaults. The key is transparency and opt-out ability.
Why do some patients still not take their meds even with nudges?
Nudges don’t work equally for everyone. Patients with depression or anxiety see 31.4% less benefit. Polypharmacy (taking five or more drugs) cuts adherence by 8.3% per additional pill. Asymptomatic conditions (like high cholesterol) reduce adherence by 32.7% because there’s no daily reminder of illness. Negative beliefs about medication cause 41.2% of discontinuations. These require deeper interventions-like counseling or simplified regimens-not just text reminders.
What’s the biggest barrier to implementing behavioral economics in healthcare?
The biggest barrier is integration. 78.3% of healthcare systems report compatibility issues with electronic health records. Staff training takes 12.7 hours per clinician. And only 34.2% of programs sustain adherence gains beyond 6 months. Cost is also a factor: smart pill bottles cost $47.50 per patient monthly, while SMS reminders cost $8.25. Sustainability requires system-wide support-not just pilot programs.