Xeloda vs. Alternative Chemotherapy Comparison Tool
Recommended Treatment Based on Your Criteria
Detailed Comparison:
When doctors talk about oral chemotherapy, the name Xeloda alternatives pops up a lot. Patients diagnosed with colorectal, breast, or gastric cancers often wonder: is Xeloda the right choice for me, or should I look at other pills on the market? This guide breaks down Xeloda (capecitabine) side‑by‑side with the most common alternatives, so you can see how they stack up on efficacy, safety, convenience, and cost.
Key Takeaways
- Xeloda is an oral pro‑drug that transforms into 5‑fluorouracil (5‑FU) inside tumor cells, offering similar effectiveness with a more convenient pill form.
- Alternatives such as 5‑FU (IV), S‑1, trifluridine/tipiracil (Lonsurf), and tegafur/uracil (UFT) differ in administration route, side‑effect profile, and approved cancer types.
- Patients with good kidney function and a desire to avoid frequent infusions often prefer Xeloda or other oral agents.
- Cost varies widely: generic capecitabine is usually cheaper than iv 5‑FU, while newer agents like Lonsurf can be pricier.
- Choosing the best option requires weighing tumor stage, previous therapy, comorbidities, and personal lifestyle.
What Is Xeloda (Capecitabine)?
Capecitabine is a oral fluoropyrimidine that gets converted into 5‑fluorouracil (5‑FU) once it reaches tumor tissue. It was first approved by the EMA in 2000 for metastatic colorectal cancer, and later gained approval for breast and gastric cancers. The drug is taken in two daily doses for two weeks, followed by a one‑week break (the classic 14‑day on/7‑day off schedule). Because it’s a pill, patients can avoid the central‑line placement required for IV 5‑FU, but they still need regular blood work to monitor liver and kidney function.
Major Oral and IV Alternatives
Below are the most widely used alternatives to Xeloda. Each has its own strengths, and the right choice often depends on the specific cancer type and patient health.
1. 5‑Fluorouracil (5‑FU) - Intravenous
5‑Fluorouracil is a cornerstone IV chemotherapy that directly delivers the active drug into the bloodstream. It works by blocking DNA synthesis in rapidly dividing cells. The most common regimens are a continuous 48‑hour infusion (the “bolus” method) or a weekly short infusion.
Pros:
- Well‑studied with decades of data on response rates.
- Can be combined with leucovorin to boost efficacy.
- Requires a hospital visit or infusion pump.
- Higher risk of acute toxicities like severe neutropenia.
2. S‑1 - Oral Combination
S‑1 blends tegafur (a 5‑FU pro‑drug) with two modulators - gimeracil and oteracil - to enhance cancer kill and reduce gut toxicity. It’s licensed in Japan, Korea, and some European countries for gastric and colorectal cancers.
Pros:
- Higher bioavailability than capecitabine in some Asian populations.
- Lower incidence of hand‑foot syndrome.
- Limited availability outside Asia.
- Requires dose adjustments based on body surface area.
3. Trifluridine/Tipiracil (Lonsurf) - Oral
Trifluridine/Tipiracil combines a nucleoside analog (trifluridine) with a thymidine phosphorylase inhibitor (tipiracil) to increase drug exposure. It’s approved for metastatic colorectal cancer after failure of standard therapies, and for gastric cancer in later lines.
Pros:
- Effective in heavily pre‑treated patients.
- Convenient once‑daily dosing.
- Typically more expensive than generic capecitabine.
- Common side effects include neutropenia and fatigue.
4. Tegafur/Uracil (UFT) - Oral
Tegafur/Uracil pairs the 5‑FU pro‑drug tegafur with uracil, which blocks dihydropyrimidine dehydrogenase (DPD) to increase 5‑FU levels. UFT is used in several Asian countries for colorectal and gastric cancers.
Pros:
- Lower peak plasma concentrations reduce acute toxicities.
- Can be taken with food, easing gastrointestinal upset.
- Less data in Western populations.
- May require more frequent dosing (typically three times daily).
How We Compare These Drugs
To give you a clear picture, we evaluated each option across five key dimensions that matter most to patients and clinicians.
- Efficacy: Objective response rate (ORR) and progression‑free survival (PFS) from major phaseIII trials.
- Safety profile: Frequency of Grade3‑4 toxicities, especially hand‑foot syndrome, neutropenia, and diarrhea.
- Convenience: Route of administration, dosing frequency, and need for central‑line or infusion pump.
- Cost: Approximate UK NHS drug‑tariff price per treatment cycle (2024‑25 data).
- Regulatory approval: Indications covered in the UK and EU.
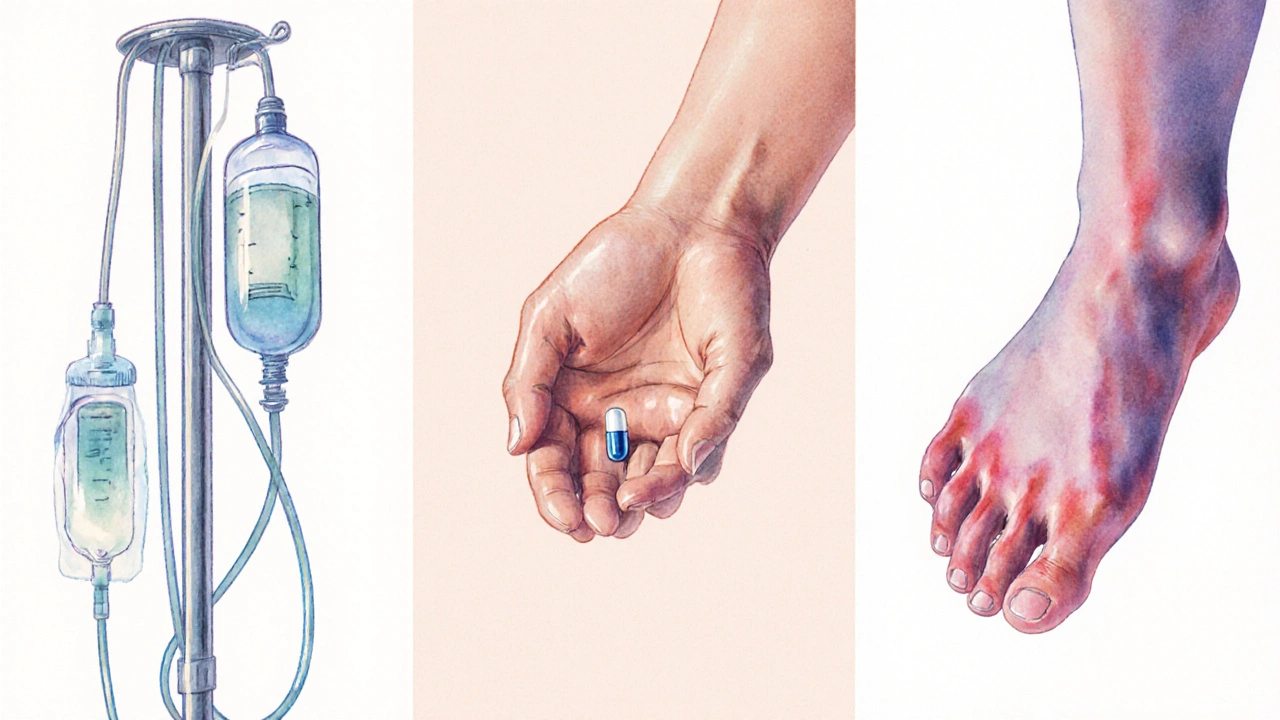
Side‑Effect Spotlight: Hand‑Foot Syndrome
One of the most talked‑about toxicities for oral fluoropyrimidines is hand‑foot syndrome, a painful redness and swelling of the palms and soles. Capecitabine and UFT have the highest reported rates (up to 30% of patients experience Grade2‑3), while S‑1 tends to be gentler (≈10%). Lonsurf rarely causes this skin reaction, but it can lead to severe neutropenia in up to 20% of patients.
Quick Comparison Table
| Drug | Route | Typical Dose | Approved Indications (UK) | ORR / PFS (median) | Common Grade3‑4 Toxicities | Approx. Cost per 3‑week Cycle (GBP) |
|---|---|---|---|---|---|---|
| Capecitabine (Xeloda) | Oral | 1250mg/m² twice daily (14days on/7days off) | Metastatic colorectal, breast, gastric | ~20% ORR; PFS 5‑7months | Hand‑foot, diarrhea, neutropenia | ≈£650 |
| 5‑Fluorouracil | IV infusion | 400mg/m² bolus + 2400mg/m² 46‑hr infusion | Colorectal, gastric, head & neck | ~25% ORR; PFS 6‑8months | Neutropenia, mucositis, cardiac toxicity | ≈£720 (incl. infusion set) |
| S‑1 | Oral | 40‑60mg/m² daily (4weeks on/2weeks off) | Gastric, colorectal (Asia) | ~22% ORR; PFS 6‑9months | Diarrhea, neutropenia, low hand‑foot | ≈£780 (imported) |
| Trifluridine/Tipiracil (Lonsurf) | Oral | 35mg/m² twice daily (2weeks on/1week off) | Metastatic colorectal (post‑standard), gastric | ~5% ORR; PFS 2‑3months (late line) | Neutropenia, fatigue, anemia | ≈£2,200 |
| Tegafur/Uracil (UFT) | Oral | 300mg/m² per day (divided 3×) | Colorectal, gastric (Asia) | ~18% ORR; PFS 5‑6months | Diarrhea, mild hand‑foot, nausea | ≈£540 |
Decision Guide: Which Drug Fits Your Situation?
Below is a quick rule‑of‑thumb matrix. Match your personal health factors to the drug that scores highest on the dimensions that matter most to you.
- Prefer oral and want fewer hospital visits? Capecitabine or S‑1 are top choices. If hand‑foot is a concern, S‑1 may be gentler.
- Have severe kidney impairment (eGFR <30mL/min)? Avoid capecitabine; consider IV 5‑FU with dose reduction.
- Already failed standard 5‑FU/oxaliplatin regimens? Lonsurf is specifically approved for that setting.
- Budget‑sensitive and live in the UK? Generic capecitabine or UFT (if available) provide the best price‑performance ratio.
- Concerned about hand‑foot syndrome? Lonsurf and S‑1 show the lowest incidence.
Practical Checklist Before Starting Therapy
- Confirm cancer type and stage with your oncology team.
- Get baseline labs: CBC, liver enzymes, renal function, and DPD activity (if available).
- Discuss pill burden and schedule - can you manage twice‑daily dosing?
- Ask about supportive care: moisturizers for hand‑foot, anti‑diarrheal meds, and growth‑factor support.
- Review NHS formulary pricing and any patient access schemes.
- Set up a clear follow‑up plan: weekly blood tests for the first two cycles, then every two weeks.
Frequently Asked Questions
Frequently Asked Questions
Can I switch from IV 5‑FU to capecitabine mid‑treatment?
Yes, many oncologists transition patients to capecitabine after an initial response to IV 5‑FU, especially if vascular access is problematic. The switch usually follows a wash‑out period of 1‑2weeks to avoid overlapping toxicity.
What if I develop severe hand‑foot syndrome on Xeloda?
First, stop the drug temporarily and start a steroid cream or urea‑based emollient. Dose reduction to 75% is common once symptoms improve. In extreme cases, clinicians may switch to an alternative like S‑1 or Lonsurf.
Is capecitabine safe during pregnancy?
No. Like all fluoropyrimidines, capecitabine is teratogenic and classified as Pregnancy Category D. Effective contraception is mandatory during treatment and for at least three months after the last dose.
How does insurance coverage differ between Xeloda and Lonsurf?
In the UK, capecitabine is listed on the NHS Cancer Drugs Fund and generally covered without extra paperwork. Lonsurf, being newer and more expensive, often requires a specialist prescribing form and justification of previous treatment failure.
Can I take capecitabine with other oral cancer drugs?
Combination therapy is common (e.g., capecitabine + bevacizumab). However, avoid concurrent use with other fluoropyrimidines or strong CYP3A4 inducers without dose adjustment, as this can raise toxicity risk.
Wrapping Up
Choosing between Xeloda and its alternatives isn’t a one‑size‑fits‑all decision. By looking at efficacy, side‑effects, how the drug is taken, and the real cost to the NHS or private patient, you can match the regimen to your life and health status. Keep this guide handy, talk openly with your oncology team, and remember that regular monitoring is key to catching any problem early.
