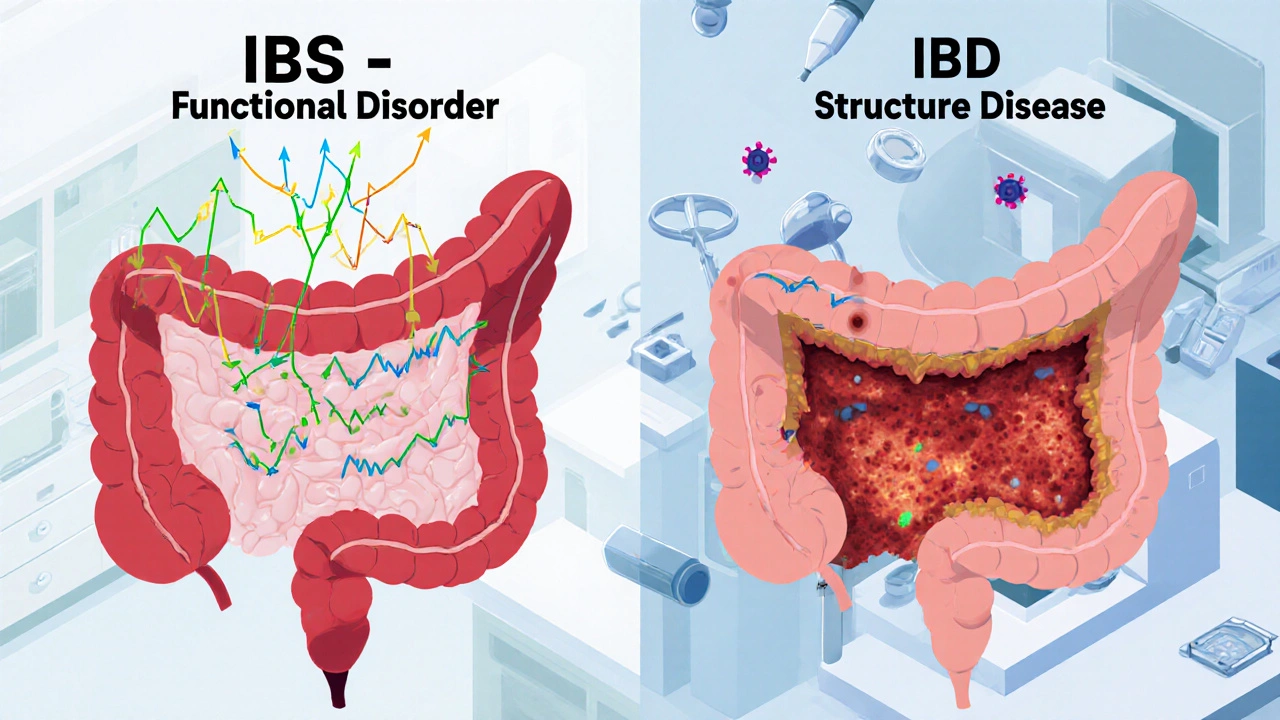
Many people think IBS and IBD are the same thing because both cause belly pain, bloating, and changes in bowel habits. But they’re not. One is a functional disorder, the other is a structural disease. Mixing them up can lead to wrong treatments, unnecessary stress, or worse - missing something serious.
What Is IBS?
IBS stands for Irritable Bowel Syndrome. It’s not caused by inflammation, ulcers, or damage to your intestines. Your colon looks perfectly normal on a colonoscopy. No tumors. No bleeding. No scarring. But it doesn’t work right.
Think of it like a misfiring engine. Everything’s intact, but the signals are off. Your gut muscles contract too strongly or too weakly. Your nerves become hypersensitive. Even normal gas or food movement can feel like cramping or pain.
The Rome IV criteria - the gold standard for diagnosis - say you must have abdominal pain at least one day a week for three months, along with two or more of these:
- Pain that improves after a bowel movement
- Changes in how often you go
- Changes in stool appearance
Most people with IBS fall into one of three types: diarrhea-predominant (IBS-D), constipation-predominant (IBS-C), or mixed (IBS-M). About 76% report bloating. Nearly half notice mucus in their stool. Symptoms often flare after eating - especially foods high in FODMAPs like onions, garlic, beans, or dairy.
Here’s what IBS is NOT:
- It doesn’t cause blood in your stool.
- It doesn’t lead to weight loss unless you’re avoiding food out of fear.
- It doesn’t raise your fever.
- It doesn’t increase your risk of colon cancer.
Doctors diagnose IBS by ruling everything else out. Blood tests, stool tests, colonoscopies - they all come back normal. If you have alarm signs like unexplained weight loss, rectal bleeding, or a family history of colorectal cancer, you’re not being tested for IBS. You’re being tested for something else.
What Is IBD?
IBD - Inflammatory Bowel Disease - is not one condition. It’s two: Crohn’s disease and ulcerative colitis. Both involve chronic, visible inflammation that eats away at your digestive tract.
In ulcerative colitis, inflammation starts in the rectum and creeps up the colon. The lining becomes red, swollen, and covered in ulcers. In Crohn’s disease, inflammation can hit anywhere - mouth to anus - and it goes deeper, affecting all layers of the bowel wall. That’s why Crohn’s can cause fistulas (abnormal tunnels between organs) and strictures (narrowing from scar tissue).
These aren’t just uncomfortable. They’re dangerous. About 92% of ulcerative colitis patients have bloody stools. In Crohn’s, 15% develop melena - black, tarry stools from upper GI bleeding. Weight loss? Common. Fever? Frequent during flares. Joint pain, eye inflammation, skin rashes? All possible. These are called extraintestinal manifestations. They don’t happen in IBS.
Diagnostic tests for IBD don’t lie:
- Colonoscopy shows ulcers, bleeding, and inflamed tissue - biopsies confirm it.
- Fecal calprotectin levels above 250 µg/g? Almost always IBD. Normal in IBS.
- C-reactive protein (CRP) over 5 mg/L? Inflammation. IBS patients stay under 3.
- MRI or CT scans show thickened bowel walls, abscesses, or fistulas - signs you won’t see in IBS.
IBD can lead to serious complications. After 10 years of pancolitis (ulcerative colitis affecting the whole colon), your risk of colorectal cancer rises by 2% each year. Toxic megacolon - a life-threatening dilation of the colon - happens in 2-4% of severe cases. These aren’t theoretical risks. They’re real, documented outcomes.
The Key Difference: Damage vs. Dysfunction
The biggest confusion comes from thinking IBS and IBD are on a spectrum. They’re not. They’re different categories entirely.
IBS = functional. Like a computer running slow because of bad software. No hardware damage. Just miscommunication.
IBD = structural. Like a house with a leaking roof, rotting beams, and mold. The damage is visible. It needs repair.
That’s why treatments are worlds apart.
IBS treatment focuses on calming the gut and managing triggers:
- Low-FODMAP diet - reduces symptoms in 76% of patients.
- Low-dose antidepressants (like amitriptyline) - help with pain and bowel control.
- Eluxadoline or rifaximin - for IBS-D.
- Probiotics and fiber - some help, some don’t. It’s individual.
IBD treatment fights inflammation:
- Anti-TNF drugs (infliximab, adalimumab) - block the body’s inflammatory signals. About half of Crohn’s patients go into remission within 14 weeks.
- Corticosteroids - quick relief for flares, but not for long-term use due to side effects.
- Vedolizumab - targets gut-specific inflammation. Works in nearly half of ulcerative colitis patients after a year.
- Surgery - sometimes needed for strictures, fistulas, or uncontrolled bleeding.
And here’s something many don’t know: You can have both. About 22-35% of people with IBD in remission still meet the criteria for IBS. Their gut is healed, but the nerves are still overreacting. That’s why treating IBD doesn’t always fix all symptoms - you might need IBS management on top of it.
When to See a Doctor
Not every belly ache needs a colonoscopy. But some signs are red flags you can’t ignore:
- Blood in your stool - never normal.
- Unexplained weight loss - especially if you’re eating normally.
- Constant fever - not from a cold or flu.
- Severe, persistent pain that wakes you up at night.
- Family history of IBD or colorectal cancer.
If you have these, don’t assume it’s IBS. See a doctor. Get blood work. Get a stool test. Get a colonoscopy if needed. IBD doesn’t wait. Early treatment changes outcomes.
And if you’ve been told you have IBS but keep having symptoms like fever or weight loss - get a second opinion. You might have been misdiagnosed.
Living With Either Condition
Both IBS and IBD can wreck your life. People with IBS say they’d give up caffeine, sex, or even their phone to be free of symptoms. IBD patients face hospitalizations, surgeries, and lifelong medication.
But the prognosis is different. IBS doesn’t shorten your life. It doesn’t cause cancer. It’s frustrating, but not deadly.
IBD can. That’s why tracking your symptoms matters. Keeping a journal of pain, stool changes, diet, and stress helps your doctor spot patterns. It also helps you know when it’s time to escalate care.
There’s no cure for either. But for IBD, remission is possible. For IBS, control is achievable. The key is knowing which one you have - and treating it accordingly.

Common Myths Debunked
Myth: IBS turns into IBD.
Truth: It doesn’t. Not ever. The Rome Foundation and CDC both confirm this. IBS is not a precursor to IBD.
Myth: Stress causes IBS or IBD.
Truth: Stress doesn’t cause either, but it can make symptoms worse. IBD flares are triggered by immune activity, not anxiety. IBS flares are triggered by gut-brain miscommunication - and stress can amplify that.
Myth: If your colonoscopy is normal, it’s IBS.
Truth: Not always. You could still have IBD if the inflammation is in the small intestine (Crohn’s) or if the biopsy missed the affected area. That’s why doctors look at blood tests, imaging, and symptoms together.
Myth: IBD is just "bad IBS."
Truth: No. It’s like comparing a sprained ankle to a broken leg. Both hurt. One heals. The other needs surgery.
Can IBS cause bloody stools?
No. Blood in the stool is not a symptom of IBS. If you’re seeing red or black stools, it’s a sign of inflammation, ulcers, or bleeding - all indicators of IBD or another serious condition. You need medical evaluation immediately.
Can you have both IBS and IBD at the same time?
Yes. About one in three people with IBD in remission still experience IBS-like symptoms - like bloating and abdominal pain - even when their inflammation is under control. This is called "IBD-IBS overlap." It requires a dual treatment approach: managing inflammation and addressing gut sensitivity.
Is IBD an autoimmune disease?
Yes. IBD - both Crohn’s disease and ulcerative colitis - is classified as an autoimmune condition. The immune system mistakenly attacks the lining of the digestive tract, causing chronic inflammation. IBS is not autoimmune. It’s a disorder of gut-brain communication.
Do I need a colonoscopy to diagnose IBS?
Not to diagnose IBS itself - but to rule out IBD and other conditions. Colonoscopy is part of the diagnostic process for IBS because it confirms there’s no inflammation, polyps, or cancer. If the colon looks normal and inflammatory markers are low, IBS is likely.
Can diet cure IBD or IBS?
No diet cures either condition. But the low-FODMAP diet can reduce IBS symptoms in 76% of people. For IBD, diet helps manage flares and supports nutrition, but it doesn’t replace medication. Anti-inflammatory drugs, biologics, and sometimes surgery are necessary to control IBD.
Does IBS increase cancer risk?
No. IBS does not cause structural damage to the colon and does not raise your risk of colorectal cancer. That’s a key difference from IBD, where long-standing inflammation increases cancer risk over time.
Final Takeaway
IBS and IBD look similar on the surface. But under the hood, they’re completely different. One is a software glitch. The other is hardware failure.
Getting the right diagnosis changes everything - your treatment, your prognosis, your peace of mind. If you’re tired of guessing, ask for the right tests. Push for blood work, stool tests, and imaging if symptoms are severe or worsening.
Don’t let confusion delay care. Your gut deserves clarity - not just comfort.