Diabetes GI Symptom Assessment Tool
Symptom Assessment
Select your symptoms and blood sugar patterns to identify potential gastrointestinal issues related to diabetes.
-
Feeling sick to your stomach, especially after eating
-
Forcing stomach contents out, especially undigested food
-
Frequent loose or watery stools
-
Infrequent bowel movements with hard stools
-
Burning sensation in chest or throat
-
Feeling of fullness or swelling in abdomen
-
Feeling full after eating small amounts of food
Your Potential GI Condition
Recommended Management
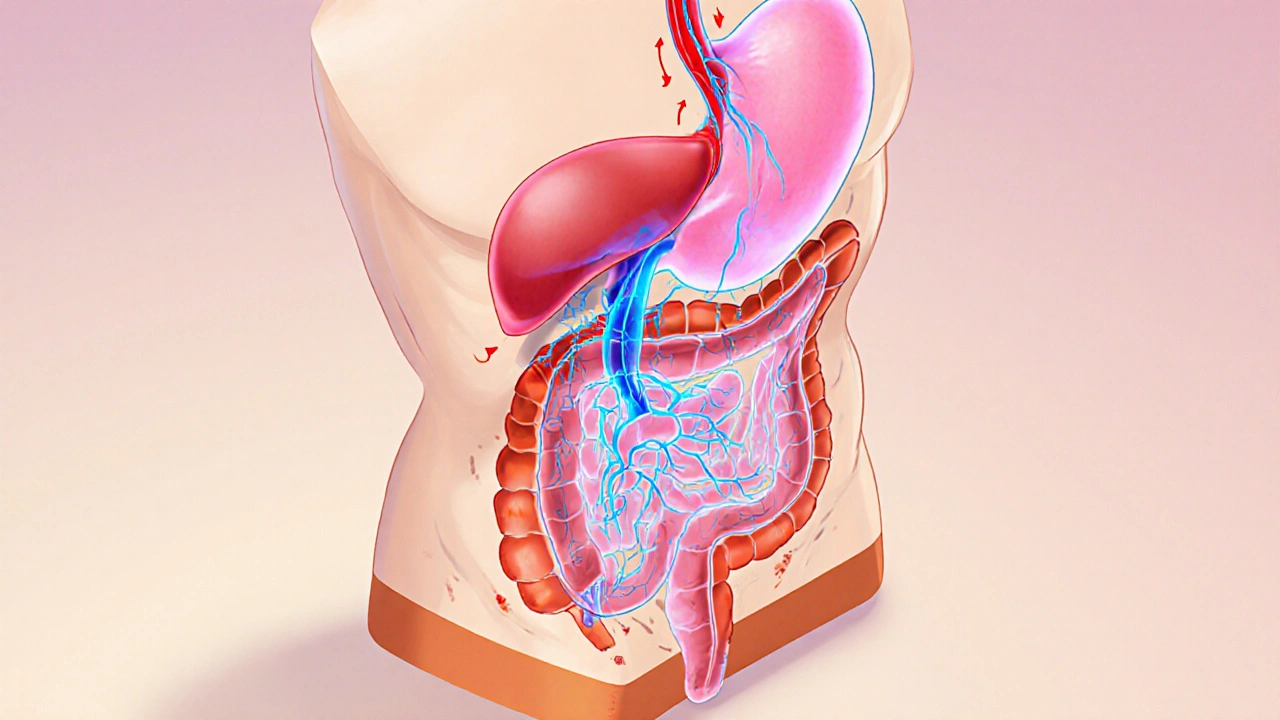
When Diabetes is a chronic metabolic disorder that raises blood sugar levels, it doesn’t stay confined to the pancreas. Over time, high glucose can mess with the nerves, muscles and blood vessels that control the gut, paving the way for a whole set of gastrointestinal issues.
Why high blood sugar messes with the gut
Glucose isn’t just a fuel for your muscles; it also powers the tiny muscles (smooth muscle) that push food through the digestive tract. When sugar spikes, two things happen:
- Elevated insulin and glucose trigger inflammation in the walls of the intestine.
- Prolonged hyperglycemia damages the autonomic nerves that tell the gut when to contract and relax.
That nerve damage is known as diabetic autonomic neuropathy. It slows down the coordinated rhythm of peristalsis, leading to both slowed and erratic movement of food.
Common gastrointestinal problems linked to Gastrointestinal Issues
People with diabetes report digestive complaints up to three times more often than those without the condition. The most frequent culprits are:
- Gastroparesis - delayed emptying of the stomach.
- Diarrhea - often unpredictable and linked to rapid transit.
- Constipation - slowed colonic motility.
- Gastroesophageal reflux disease (GERD) - acid flowing back into the esophagus.
- Irritable Bowel Syndrome‑like symptoms - bloating, cramping, and alternating bowel habits.
Each of these conditions has a slightly different mechanism, but they all trace back to the same root causes: nerve damage, altered hormone signaling, and fluctuating blood‑sugar levels.
Gastroparesis - when the stomach forgets to empty
Gastroparesis affects roughly 5‑12% of people with type 1 diabetes and 1‑5% of those with type 2. The stomach’s pacemaker cells (interstitial cells of Cajal) rely on normal autonomic input. When those signals falter, food sits in the stomach longer than it should.
Typical signs include early‑stage fullness, nausea after meals, and occasional vomiting of undigested food. Blood‑sugar control gets harder because the timing of glucose absorption becomes unpredictable.
Diarrhea and rapid transit
High glucose can increase intestinal secretion and speed up motility, leading to watery stools. Some patients also develop bacterial overgrowth because food hanging in the small intestine creates a breeding ground for microbes.
Managing this type of diarrhea often starts with tighter glucose control, a low‑fiber‑high‑soluble‑fiber diet, and sometimes a short‑course antibiotic to reset the gut flora.
Constipation - the slow‑moving side of the spectrum
When the autonomic nerves are sluggish, the colon contracts less frequently, and water reabsorption goes up, resulting in hard stools. Dehydration from high blood‑sugar levels only makes it worse.
Key tactics include staying hydrated, eating plenty of soluble fiber (like oats or psyllium), and, if needed, a low‑dose laxative prescribed by a clinician.
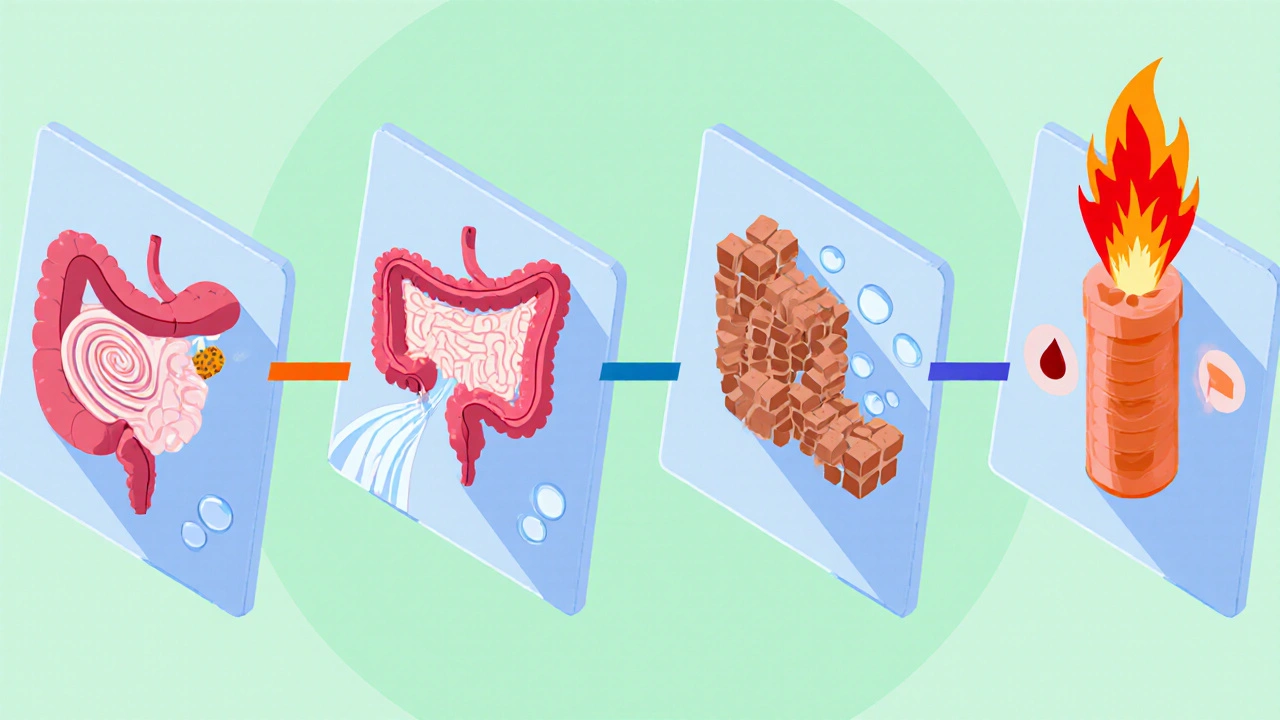
GERD - acid on the rise
Elevated intra‑abdominal pressure from delayed gastric emptying can push acid up the esophagus. In addition, certain diabetes medications relax the lower esophageal sphincter, increasing reflux risk.
Typical GERD symptoms are heartburn, sour‑taste mornings, and a chronic cough. Lifestyle tweaks (elevating the head of the bed, avoiding late‑night meals) combined with a proton‑pump inhibitor often bring relief.
IBS‑like symptoms - the confusing middle ground
Many diabetics describe alternating bouts of constipation and diarrhea, bloating, and abdominal pain. While not true IBS, the pattern mirrors it because both involve dysregulated gut‑brain signaling.
Stress reduction, a low‑FODMAP diet, and, where appropriate, a low‑dose tricyclic antidepressant can calm the gut’s nervous system.
How diabetic neuropathy fuels gut trouble
Autonomic neuropathy isn’t limited to the gut; it also impacts bladder control and heart rate variability. When you see a pattern of multiple organ systems acting up, it’s a red flag that nerve damage is spreading.
Early detection is crucial. Simple bedside tests-like checking the post‑prandial rise in blood sugar after a standardized meal-can flag delayed gastric emptying before major symptoms appear.
Practical steps to protect your digestive health
- Maintain target blood‑glucose ranges (70‑180 mg/dL for most adults). Tight control reduces nerve injury risk.
- Eat smaller, more frequent meals. This eases the workload on the stomach and steadies glucose spikes.
- Choose low‑glycemic carbohydrates (whole grains, legumes) to avoid rapid glucose surges.
- Stay hydrated - aim for at least 1.5 L of water daily, more if you’re active.
- Include soluble fiber (psyllium, oats) but avoid excessive insoluble fiber if you have gastroparesis.
- Limit alcohol and caffeine, both of which can aggravate GERD.
- Schedule regular foot and eye exams - they can also reveal early autonomic changes.
- Discuss medication side‑effects with your doctor; some GLP‑1 agonists can slow gastric emptying.

When to seek medical help
If you notice any of the following, schedule an appointment promptly:
- Persistent nausea or vomiting after meals.
- Weight loss despite normal or increased appetite.
- Sudden, severe abdominal pain.
- Frequent episodes of diarrhea that interfere with daily life.
- Unexplained constipation lasting more than two weeks.
- Recurrent heartburn that doesn’t respond to over‑the‑counter meds.
Your clinician may order a gastric emptying study, an abdominal ultrasound, or specific blood tests to pinpoint the cause.
Quick checklist for daily gut‑friendly diabetes care
- Check blood sugar before and after meals.
- Log any digestive symptoms alongside glucose readings.
- Eat a balanced plate: half non‑starchy veg, a quarter lean protein, a quarter low‑GI carbs.
- Move after meals - a gentle 10‑minute walk can stimulate motility.
- Hydrate - sip water throughout the day, not just with meals.
- Review meds every 6 months for possible gut side‑effects.
Frequently Asked Questions
Can type 1 diabetes cause more gut problems than type 2?
Both types can lead to gastrointestinal issues, but type 1 often shows up earlier and may be linked to a higher prevalence of gastroparesis because the disease usually starts at a younger age and can be harder to keep blood sugar stable.
Is it safe to eat fiber if I have gastroparesis?
Soluble fiber (like psyllium) is usually well‑tolerated because it forms a gel that moves slowly. Insoluble fiber (raw veggies, whole nuts) can linger and worsen bloating, so it’s best to limit those.
Do diabetes medications affect gut motility?
Yes. Some GLP‑1 receptor agonists (e.g., exenatide, semaglutide) intentionally slow gastric emptying to lower post‑meal glucose spikes, which can exacerbate nausea or gastroparesis in susceptible people.
How is diabetic gastroparesis diagnosed?
A gastric emptying scintigraphy is the gold‑standard test. It measures how quickly a radiolabelled meal leaves the stomach over a four‑hour period. Alternatives include a breath test using carbon‑13‑labeled meals or an endoscopic ultrasound.
Can probiotics help with diabetes‑related diarrhea?
Probiotics that contain Lactobacillus or Bifidobacterium strains can restore a healthy balance in the small intestine, reducing bacterial overgrowth and easing loose stools. Choose a product with at least 5 billion CFU per dose and take it with meals.
Comparison of common GI complications in diabetes
| Condition | Typical Prevalence in Diabetes (%) | Core Symptoms | First‑Line Management |
|---|---|---|---|
| Gastroparesis | 5‑12 (type 1), 1‑5 (type 2) | Early satiety, nausea, vomiting, erratic glucose spikes | Dietary modification (small, low‑fat meals), prokinetic agents (metoclopramide), blood‑sugar optimization |
| Diarrhea (rapid transit) | ≈15 | Watery stools, urgency, possible bloating | Glucose control, soluble fiber, occasional antibiotics for SIBO |
| Constipation | ≈20 | Hard stools, infrequent bowel movements, abdominal discomfort | Hydration, soluble fiber, osmotic laxatives if needed |
| GERD | ≈30 | Heartburn, sour taste, chronic cough | Elevate head of bed, avoid late meals, PPIs or H2 blockers |
| IBS‑like symptoms | ≈25 | Bloating, alternating constipation/diarrhea, pain | Low‑FODMAP diet, stress management, low‑dose tricyclics |