Anticoagulant Restart Timing Calculator
Calculate Safe Restart Time
This tool helps determine the appropriate time to safely restart anticoagulants after epidural or spinal procedures based on ASRA guidelines.
Recommended Restart Time
When you're on blood thinners and need an epidural or spinal procedure-whether for labor, chronic back pain, or surgery-the biggest fear isn't the needle. It's the hematoma. A rare but devastating complication that can turn a routine procedure into a life-altering event. This isn't theoretical. In the U.S. alone, over 40 million spinal procedures are done each year. And for patients on anticoagulants, the stakes are real.
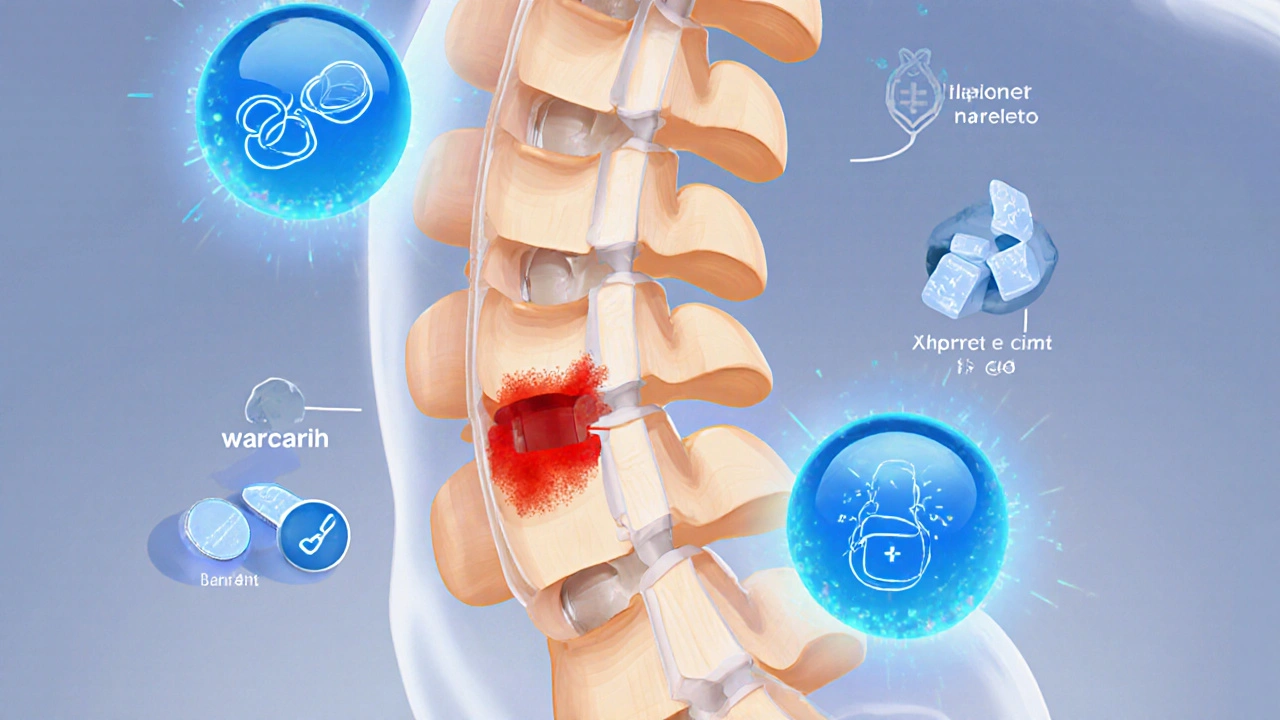
What Exactly Is a Spinal Epidural Hematoma?
A spinal epidural hematoma (SEH) happens when blood leaks into the space between the spinal cord’s protective membrane (the dura) and the ligament that runs along the spine. Even a tiny amount-just 1 to 2 milliliters-can compress the spinal cord. That’s less than half a teaspoon. Because the spinal canal is so narrow, that small pool of blood can crush nerves, leading to paralysis, loss of bladder control, or permanent nerve damage. It doesn’t always show up right away. Symptoms usually hit within 12 hours: sharp pain in the middle of your back, numbness in your legs, weakness in your feet, or trouble peeing. If you feel any of these after a spinal procedure while on blood thinners, don’t wait. Every minute counts. Studies show that patients who get surgery within 8 hours have a 79% chance of full recovery. After 24 hours? That drops to 9%.Which Blood Thinners Carry the Highest Risk?
Not all anticoagulants are created equal. Your risk depends on the drug you’re taking, how much, and when you took it last.- Warfarin: Risk spikes if your INR (a blood test that measures clotting) is above 1.4. At that level, your risk jumps 8.7 times compared to someone with normal clotting. Even if your INR is normal, there are documented cases of hematomas-so don’t assume you’re safe just because your lab result looks good.
- Low Molecular Weight Heparin (LMWH): Think Lovenox or enoxaparin. If you take a therapeutic dose (for clots), you need to stop it at least 24 hours before the procedure. Prophylactic doses (lower, for prevention) still need a 10-12 hour gap. The FDA flagged over 100 cases linked to Lovenox between 1992 and 2013.
- DOACs (Direct Oral Anticoagulants): These include Xarelto (rivaroxaban), Eliquis (apixaban), and others. For people with normal kidney function, you need to stop rivaroxaban or apixaban 48 hours before the procedure. If your kidneys aren’t working well (CrCl under 50), extend that to 72 hours. Apixaban carries slightly lower risk than rivaroxaban, but both can cause hematomas if timing is off.
- Antiplatelets: Aspirin alone? Risk is extremely low-studies show almost zero cases in thousands of procedures. But if you’re on dual therapy (like aspirin + clopidogrel), your risk triples. Many doctors still advise stopping both for 7 days before surgery.
It’s Not Just the Medication-These Factors Multiply Risk
Even if you stop your blood thinner perfectly, other things can push you into danger zone:- Multiple needle attempts: If the anesthesiologist has to stick you three or more times, your risk jumps 6.2 times. That’s why experience matters.
- Bleeding during the procedure: If the fluid coming out of your spine looks bloody (blood-tinged CSF), your risk goes up 11.8 times.
- Epidural catheter vs. single shot: Leaving a catheter in place increases risk by 2.3 times compared to a one-time injection.
- Age and kidney function: If you’re over 70, your risk is 3.7 times higher. If your kidney function is below 30 mL/min, it’s 4.9 times higher.
- Spinal stenosis: Narrowed spinal canal? That’s a 2.8 times higher risk.
- Low hemoglobin or heavy bleeding: If your blood count is under 10 g/dL or you lose more than a liter during surgery, your risk doubles or triples.

Timing Is Everything-Here’s the Real Protocol
The American Society of Regional Anesthesia (ASRA) guidelines are the gold standard. But many providers still get it wrong. A 2022 survey found only 58% of pain doctors knew the correct timing rules.Here’s what actually works:
- Warfarin: Check INR within 24 hours before. Target must be under 1.4. Restart 4 hours after single injection, 6 hours after catheter removal.
- LMWH (prophylactic): Stop 10-12 hours before. Restart 2 hours after single injection, 4 hours after catheter.
- LMWH (therapeutic): Stop 24 hours before. Restart 4 hours after catheter removal.
- Rivaroxaban or Apixaban (normal kidneys): Stop 48 hours before. Restart 6-24 hours after, depending on bleeding risk.
- Rivaroxaban or Apixaban (impaired kidneys): Stop 72 hours before. Wait 24-48 hours to restart.
And never, ever skip the INR check. One case study showed a patient with INR of 1.2 still developed a hematoma. Lab numbers aren’t foolproof.
What Happens If You Ignore the Rules?
The consequences aren’t just medical-they’re financial and legal.A single spinal hematoma case costs an average of $287,450. That includes emergency surgery, months of rehab, and lifelong care if paralysis occurs. Compare that to a standard epidural steroid injection, which runs about $1,200.
In 2022, 78 malpractice claims were filed in the U.S. over spinal hematomas. Over 60% resulted in payouts averaging $1.2 million. Why? Failure to follow timing protocols (41%) or not monitoring patients closely after the procedure (37%).
The FDA now requires all anticoagulant manufacturers to include specific warnings about neuraxial procedures. Hospitals are being monitored. Starting in January 2025, any U.S. hospital doing more than 50 spinal procedures a year must report hematoma rates to federal safety agencies.
What About Newer Drugs and Emerging Science?
The field is evolving. A 2023 case report showed a hematoma after edoxaban-even after 72 hours of stopping it. That suggests our current guidelines might not cover every new drug perfectly.Researchers are now looking at blood biomarkers. A 2022 study found that a protein called GFAP in the blood, if above 0.72 ng/mL within two hours of the procedure, is 94% accurate at predicting a developing hematoma. That could lead to faster diagnosis-maybe even before symptoms show.
There’s also a puzzling trend: women are developing spinal hematomas 2.3 times more often than men, even with the same drugs and dosages. Why? No one knows yet. But it’s being studied.
What Should You Do If You’re on Blood Thinners?
Don’t panic. But do take action.- Speak up. Tell every doctor, nurse, and anesthesiologist you’re on anticoagulants-even if you think it’s obvious.
- Bring a list of all your meds, including over-the-counter aspirin or fish oil.
- Ask: “What’s the plan for stopping and restarting my blood thinner?” If they don’t have one, push for a consultation with a hematologist or pain specialist.
- Know your symptoms. If you get sudden back pain, leg weakness, or can’t urinate after a spinal procedure, tell someone immediately. Don’t wait.
- Use tools like the ASRA Anticoagulation Checklist or the free app “Neuraxial Anticoag.” But verify the version-it’s not rare for apps to have outdated info.
There’s no perfect answer. Stopping blood thinners raises your risk of stroke or pulmonary embolism. Continuing them raises your risk of paralysis. The goal isn’t to avoid the procedure-it’s to do it safely. That means teamwork: you, your doctor, your anesthesiologist, and a clear plan based on real data, not guesswork.
Bottom Line
Spinal hematomas from blood thinners are rare-but they’re preventable. The data is clear: timing, technique, and communication save lives. If you’re on anticoagulants and need a spinal procedure, don’t assume it’s routine. Ask the hard questions. Demand a plan. Your spine-and your future mobility-depend on it.Can I still get an epidural if I’m on aspirin?
Yes, in most cases. Studies involving over 1,200 procedures show no hematomas when patients continued low-dose aspirin alone. The risk is extremely low-less than 0.03%. However, if you’re on dual antiplatelet therapy (like aspirin plus clopidogrel), your risk increases significantly, and stopping for 7 days is usually recommended.
How long after a spinal procedure can I restart my blood thinner?
It depends on the drug and whether you had a single injection or a catheter. For warfarin, restart 4 hours after a single shot or 6 hours after catheter removal. For LMWH, wait 2 hours after single injection, 4 hours after catheter. For DOACs like rivaroxaban or apixaban, wait 6-24 hours, depending on bleeding risk. Always follow your provider’s specific plan.
Is a spinal hematoma always permanent?
No. If treated within 8 hours of symptom onset, 79% of patients recover fully. After 24 hours, that drops to 9%. Permanent damage-like paralysis or loss of bladder control-happens in about 24% of cases, especially if treatment is delayed. Early recognition is everything.
Do all blood thinners carry the same risk?
No. Warfarin with high INR, therapeutic-dose LMWH, and DOACs like rivaroxaban carry higher risk than aspirin alone. Risk also depends on timing. Taking enoxaparin 8 hours before a procedure carries a 0.31% risk; taking it 24 hours before drops that to 0.04%. DOACs like apixaban have slightly lower risk than rivaroxaban when timed correctly.
What should I do if I develop back pain after an epidural?
Don’t wait. Call your doctor or go to the emergency room immediately. Mention you’re on blood thinners. Symptoms like sudden back pain, leg weakness, numbness, or trouble urinating could mean a spinal hematoma. Time is critical-every hour matters. Imaging (MRI) will be needed urgently, and surgery may be required within hours to prevent permanent damage.