Glaucoma Medication Safety Checker
Medication Safety Assessment
When it comes to eye health, Antihistamines are drugs that block histamine receptors to relieve allergy symptoms can have unexpected effects on Glaucoma, a group of eye conditions that damage the optic nerve through elevated intra‑ocular pressure.
antihistamines and glaucoma may sound like an obscure pairing, but for the 300,000‑plus people in the UK with narrow‑angle glaucoma, the link can be life‑changing. Below we break down why some over‑the‑counter (OTC) allergy pills are risky, which ones are safer, and what you should do the next time a sneeze threatens your vision.
Glaucoma 101: Not All Types Are the Same
First, let’s get clear on the two major forms:
- Primary open‑angle glaucoma (POAG) accounts for roughly 70% of cases. The drainage angle is open, but the trabecular meshwork slowly becomes less efficient, leading to a gradual pressure rise.
- Narrow‑angle (or angle‑closure) glaucoma makes up about 10‑15% of cases. Here the iris is positioned so close to the cornea that any pupil dilation can physically block the drainage pathway, causing a sudden pressure spike.
Why does this matter? Most allergy meds are harmless for POAG patients, but for the narrow‑angle crowd they can trigger an acute angle‑closure attack-a true eye‑emergency that can blind you in minutes.
How Antihistamines Can Raise Eye Pressure
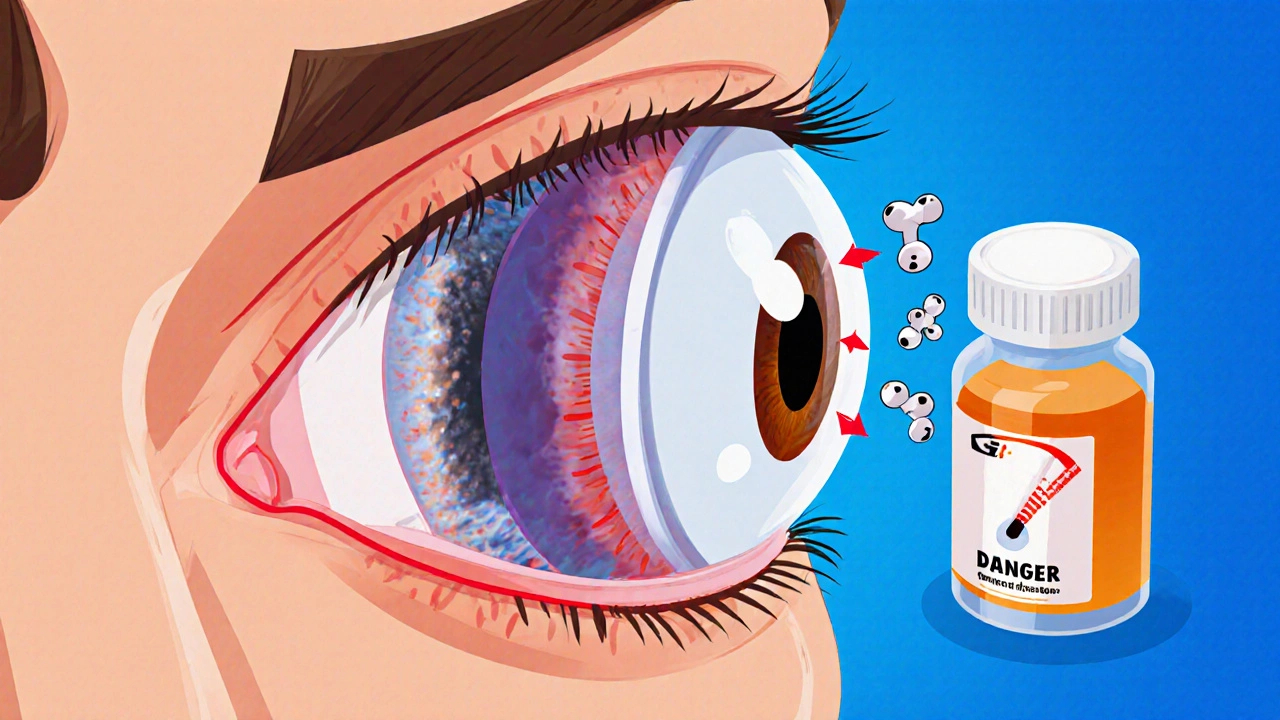
Many antihistamines have anticholinergic properties. That means they relax the muscles that keep the pupil small (the sphincter pupillae). When those muscles relax, the pupil dilates - a process called mydriasis. In a narrow‑angle eye, dilation narrows the iridocorneal angle even more, sealing off the fluid‑draining trabecular meshwork.
The result is a rapid rise in intra‑ocular pressure (IOP). Symptoms pop up fast: severe eye pain, blurry vision, halos around lights, nausea, and a red eye. If you’ve ever felt a headache after taking an allergy pill, add a pounding eye to that list, and call emergency services immediately.
Medications That Raise Risk
Not every antihistamine is created equal. Below is a quick snapshot of the most common allergy drugs and how they stack up for someone with narrow‑angle glaucoma.
| Medication | Anticholinergic? | Risk for angle‑closure | Typical OTC use |
|---|---|---|---|
| Diphenhydramine (Benadryl) | Yes - strong | High | Night‑time sleep aid, cold & allergy |
| Chlorpheniramine | Yes - moderate | Medium‑High | Allergy, cold |
| Loratadine (Claritin) | No - minimal | Low | All‑day allergy relief |
| Cetirizine (Zyrtec) | Very low | Low | Allergy, hives |
| Fexofenadine (Allegra) | No | Low | Allergy, seasonal |
| Pseudoephedrine (Sudafed) | N/A (decongestant) | Medium (vasoconstriction can raise IOP) | Nasal congestion |
| Phenylephrine nasal spray | N/A | Medium‑High (direct pupil dilator) | Nasal decongestion |
Notice the pattern: first‑generation antihistamines (diphenhydramine, chlorpheniramine) carry the biggest danger, while newer, second‑generation agents (loratadine, cetirizine, fexofenadine) are generally safer but still warrant a quick check with your eye doctor.
When Steroids Enter the Mix
Topical or oral steroids - found in some allergy eye drops, nasal sprays, and even certain cough syrups - can increase IOP even in POAG patients. The mechanism isn’t fully settled, but most experts agree that steroid‑induced protein deposits can clog the trabecular meshwork. The rule of thumb? Limit steroid‑containing allergy meds to ten days or less, and schedule a pressure check afterward.
Safer Alternatives for Allergy Relief
If you have narrow‑angle glaucoma, here’s a practical toolbox:
- Pick a second‑generation antihistamine. Loratadine (non‑sedating, minimal anticholinergic activity) or Cetirizine are good starting points.
- Avoid oral decongestants with strong vasoconstrictive effects. If you need nasal relief, saline rinses or a nasal steroid spray used short‑term under doctor supervision is safer than pseudoephedrine.
- Consider non‑drug options: HEPA air filters, allergen‑proof bedding, and keeping windows closed on high‑pollen days can cut the need for medication.
- If you must use a first‑generation antihistamine for an emergency, have a copy of your glaucoma diagnosis on hand and know the nearest emergency eye‑care center.
Practical Steps Before You Reach for the Medicine Cabinet
Follow this quick checklist the next time you feel a sneeze coming on:
- Verify your exact glaucoma diagnosis - ask your ophthalmologist to write it down (e.g., “narrow‑angle glaucoma, stage 1”).
- Read every OTC label. Look for the words “anticholinergic”, “first‑generation antihistamine”, or “phenylephrine”.
- Ask your pharmacist for a low‑risk alternative. Mention the word “glaucoma” - most will suggest loratadine or cetirizine.
- Keep a small card in your wallet that lists your glaucoma type and a warning: “Avoid diphenhydramine, chlorpheniramine, phenylephrine”.
- If you experience sudden eye pain, visual halos, or nausea after taking any medication, call emergency services and tell them you have glaucoma.
When to Seek Emergency Care
Acute angle‑closure glaucoma is a medical emergency. Here’s what to look for:
- Severe, throbbing eye pain, often with headache.
- Rapid vision loss, especially blurry or “rain‑bow” halos around lights.
- Redness of the eye, nausea, vomiting.
- Mid‑dilated pupil that does not react to light.
If any of these pop up within hours of taking an allergy pill, go to the ER. Treatment usually involves pressure‑lowering eye drops, oral carbonic anhydrase inhibitors, and a laser peripheral iridotomy to create a permanent opening in the iris.

Emerging Research & What the Future Holds
Scientists are not standing still. A 2023 clinical trial (NCT04876321) is testing a modified‑release loratadine designed to stay out of the eye, cutting any residual anticholinergic exposure. Meanwhile, several studies suggest oral statins may slow progression of open‑angle glaucoma, offering a potential dual benefit for patients who also manage cholesterol.
Regulators are catching up, too. Advocacy groups like Glaucoma UK have petitioned the UK MHRA since 2022 to add clear glaucoma warnings on OTC antihistamine packaging. Although the rule isn’t final yet, many manufacturers are voluntarily updating labels with “may increase intra‑ocular pressure in narrow‑angle glaucoma”.
In practice, the biggest change is awareness. Routine eye exams now often include gonioscopy (a quick angle‑viewing test) for anyone over 40. Early identification of a narrow angle gives you the chance to steer clear of risky meds before an accidental episode occurs.
Bottom Line Checklist
- Know your exact glaucoma type - narrow‑angle = high risk.
- Skip first‑generation antihistamines (diphenhydramine, chlorpheniramine).
- Prefer second‑generation antihistamines (loratadine, cetirizine, fexofenadine).
- Avoid oral decongestants with phenylephrine or pseudoephedrine unless approved by your doctor.
- Limit steroid‑containing allergy meds to ≤10 days and schedule IOP checks.
- Carry a medical ID or card stating your glaucoma status.
- Seek emergency care at the first sign of acute eye pain or visual halos.
Frequently Asked Questions
Can I take Claritin if I have narrow‑angle glaucoma?
Claritin (loratadine) is a second‑generation antihistamine with very low anticholinergic activity, so it’s generally considered safe for narrow‑angle patients. Still, talk to your ophthalmologist before starting any new drug.
Why do first‑generation antihistamines cause mydriasis?
They block muscarinic receptors in the eye’s sphincter muscle. When that muscle relaxes, the pupil dilates, narrowing the drainage angle in susceptible eyes.
Are nasal steroid sprays safe for glaucoma?
Short‑term use (under 10 days) is usually fine, but prolonged exposure can raise eye pressure. Have your eye pressure checked if you need steroids for more than a couple of weeks.
What should I do if I accidentally take diphenhydramine?
Monitor for sudden eye pain, halos, nausea, or visual blur. If any appear, go to the emergency department immediately and tell staff you have glaucoma.
Do statins really help with glaucoma?
Two 2022 studies found that regular statin users had a modest reduction in open‑angle glaucoma progression. They’re not a treatment on their own, but the data is encouraging for patients already on cholesterol medication.
